What Are SGLT-2 Inhibitors and How Can They Help Your Heart?
.png) By Mary Barna Bridgeman
By Mary Barna Bridgeman
SGLT-2 inhibitors can protect your heart! This type of medicine is recommended for people with type 2 diabetes who have heart disease or risk factors related to heart disease. Learn about the use of these medicines, including side effects, their effect on A1C, and their role in supporting heart health
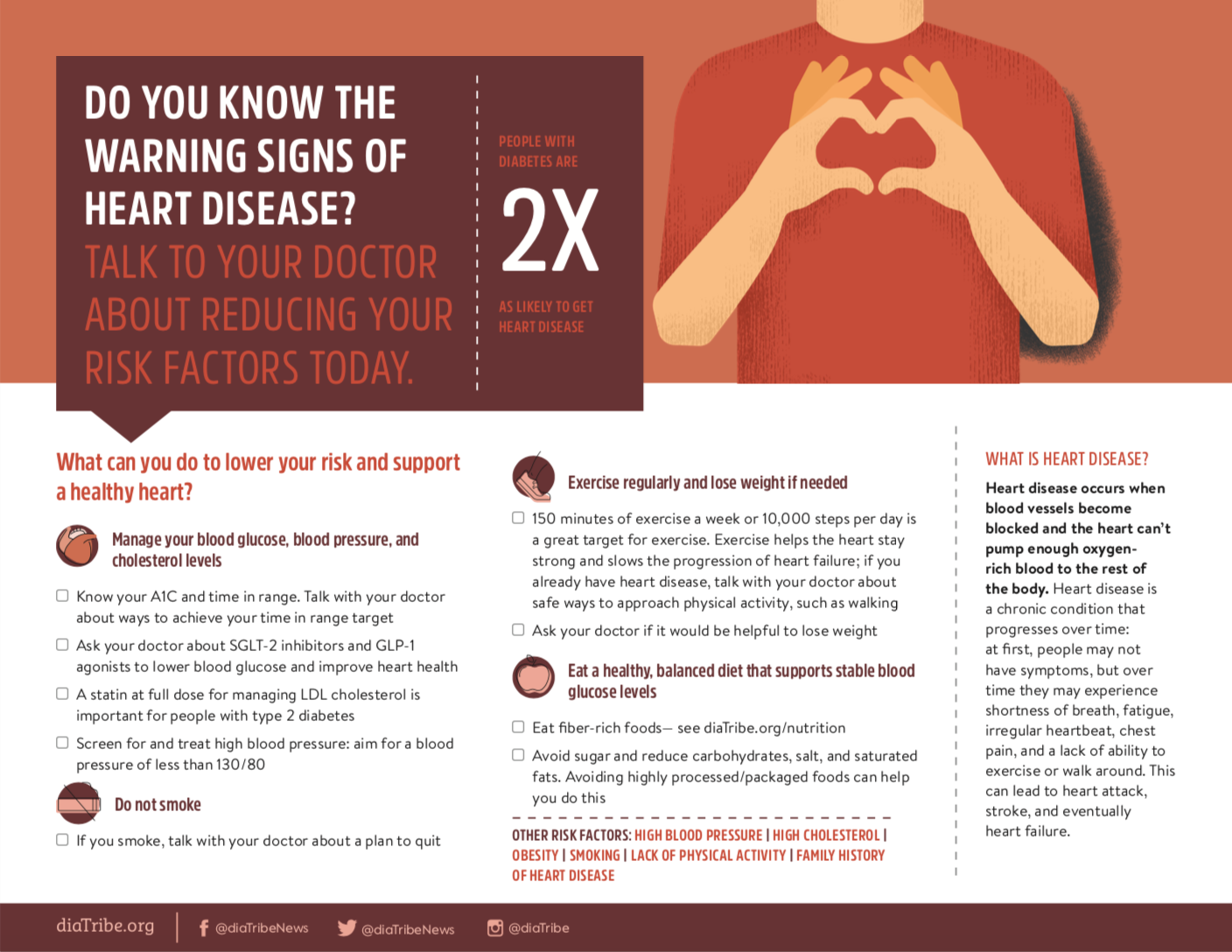
Diabetes is a risk factor for heart disease: people with diabetes are twice as likely to have heart disease or a stroke compared to those without diabetes. Heart disease is often a “silent” condition, meaning that symptoms are not necessarily present until a heart attack or a stroke actually happens. It is important for people with diabetes to realize they may be at risk – click to read more about the link between diabetes and heart disease from Know Diabetes By Heart.
There are many ways to take care of your heart and to reduce the risk of heart disease while living with diabetes. New medicines, including sodium-glucose cotransport 2 (SGLT-2) inhibitors and glucagon-like peptide-1 (GLP-1) agonists, have been shown to protect the heart and reduce the risk of many specific heart-related outcomes. This article will focus on SGLT-2 medications, and our next article will focus on GLP-1 medications.
Click to view and download diaTribe's helpful infographic on preventing heart disease.
What are SGLT-2 inhibitors?
There are currently four medicines that are categorized as SGLT-2 inhibitors:
These medicines help people with type 2 diabetes manage their glucose levels: they work in the kidneys to lower sugar levels by increasing the amount of sugar that is passed in the urine. SGLT-2s increase time in range and reduce A1C levels while also lowering blood pressure and supporting weight loss. For people with diabetes who have had a heart attack or are at high risk of heart disease, or who have kidney disease or heart failure, these medicines could be considered regardless of A1C level. While SGLT-2 medications are expensive, some assistance programs are available to help with cost – see one of diaTribe’s most popular articles, “How to Get Diabetes Drugs For Free.”
What do you need to know about SGLT-2 inhibitors?
SGLT-2s have a low risk of causing hypoglycemia (low blood sugar levels). Because they increase sugar in the urine, side effects can include urinary tract infections and genital yeast infections in men and women. Dehydration (loss of fluid) and low blood pressure can also occur. Symptoms of dehydration or low blood pressure may include feeling faint, lightheaded, dizzy, or weak, especially upon standing.
Before starting an SGLT-2 inhibitor, here are some things to discuss with your healthcare team if you have type 2 diabetes:
-
How much water to drink each day
-
Ways to prevent dehydration and what to do if you cannot eat or you experience vomiting or diarrhea (these are conditions that may increase your risk of developing dehydration)
-
Any medicines you take to treat high blood pressure
When prescribed for people with type 2 diabetes, SGLT-2s rarely cause diabetic ketoacidosis (DKA), a serious and potentially life-threatening condition. For people with type 1 diabetes, DKA is a well-known risk when SGLT-2s are prescribed. Call your healthcare professional if you have warning signs of DKA: high levels of ketones in your blood or urine, nausea, vomiting, lack of appetite, abdominal pain, difficulty breathing, confusion, unusual fatigue, or sleepiness. When you are sick, vomiting, have diarrhea, or cannot drink enough fluids, you should follow a sick day plan – see Dr. Fran Kaufman’s article on developing your sick day management plan. Your healthcare professional may instruct you to test your urine or blood ketones and stop taking your medication until symptoms go away.
If you have type 1 diabetes or chronic kidney disease, depending on your level of kidney function, these medicines may not be for you.
SGLT-2 inhibitors are usually taken as a pill once a day – often in the morning before breakfast – and can be taken with or without food.
What do SGLT-2 inhibitors have to do with heart health?
Results from clinical studies suggest SGLT-2 inhibitors may play an important role in lowering heart disease risks.
Jardiance was the first SGLT-2 inhibitor to show positive effects on heart health in the EMPA-REG OUTCOME trial. In this study, more than 7,020 adults with type 2 diabetes and a history of heart disease were followed. Participants received standard treatment for reducing heart disease risk – including statin medications, blood pressure-lowering drugs, aspirin, and other medicines – and diabetes care, plus treatment with Jardiance. Over a four-year period, results from the study showed that, compared to placebo (a “nothing” pill), Jardiance led to:
-
a 14% reduction in total cardiovascular events (heart attacks, strokes, heart-related deaths)
-
a 38% reduction in risk of heart-related death
-
a 32% reduction in overall death
-
a 35% reduction in hospitalizations from heart failure
Read diaTribe’s article on the results here.
Similarly, the heart protective effects of Invokana have been shown in two clinical studies, CANVAS and CANVAS-R. These two studies enrolled more than 10,140 adults with type 2 diabetes and a high risk of heart disease, randomly assigned to receive either Invokana or placebo treatment. In the CANVAS studies, treatment with Invokana led to the following:
-
a 14% reduction in total cardiovascular events (heart attacks, strokes, heart-related deaths)
-
a 13% reduction in risk of heart-related death
-
a 13% reduction in overall death
-
a 33% reduction in hospitalizations from heart failure
Read diaTribe’s article on the results here.
Farxiga may also reduce heart disease risks. In the DECLARE-TIMI 58 study, more than 17,000 people with type 2 diabetes received Farxiga; 40% of participants had known heart disease and 60% had risk factors for heart disease. Importantly, more than half of the people included in this study did not have existing heart disease. While Farxiga was not found to significantly reduce total cardiovascular events (heart attacks, strokes, heart-related deaths) compared with placebo, its use did lead to a 17% lower rate of heart-related death or hospitalization for heart failure. Read diaTribe’s article about the results here.
More recently, the DAPA-HF study evaluated the use of Farxiga for treating heart failure or death from heart disease in people with or without type 2 diabetes. The study included more than 4,700 people with heart failure; about 42% of those enrolled had type 2 diabetes. Farxiga was shown to reduce heart-related death or worsening heart failure by 26% compared to placebo, both in people with type 2 diabetes or without diabetes. Learn more about these results here.
Additionally, on May 26th, the FDA approved a dual SGLT-2/SGLT-1 inhibitor, sotagliflozin, to treat all types of heart failure. This medication, which will be sold under the brand name Impefa, is expected to be available around the end of June 2023.
All of the available SGLT-2 inhibitors have evidence suggesting benefits of this class of medications for people with established heart failure. Click to read diaTribe’s article on SGLT-2 Steglatro and heart health.
Other possible benefits of SGLT-2 inhibitors
Invokana, Farxiga, and Jardiance have also been shown to reduce the progression of kidney disease. Learn more about diabetes and kidney disease here.
SGLT-2s have been studied in people with type 1 diabetes, but are not yet approved for use by the FDA – you can learn about SGLT-2s for people with type 1 diabetes here.
What’s the bottom line?
You can reduce your risk of heart disease and promote heart health while living with diabetes. You and your healthcare team should develop a personalized plan to determine what ways are best for reducing your risk of heart disease. According to the latest evidence and treatment recommendations, SGLT-2 inhibitors may be most useful for people with type 2 diabetes and heart disease or at high risk of heart disease.
About Mary
Mary Barna Bridgeman, PharmD, BCPS, BCGP is a Clinical Professor at the Ernest Mario School of Pharmacy at Rutgers University. She practices as an Internal Medicine Clinical Pharmacist at Robert Wood Johnson University Hospital in New Brunswick, New Jersey.
This article is part of a series to help people with diabetes learn how to support heart health, made possible in part by the American Heart Association and American Diabetes Association’s Know Diabetes by Heart initiative.