Want to Stay Active or Get More Exercise? Strategies for Glucose Management
 By Sophie Skallerud and Kira Wang
By Sophie Skallerud and Kira Wang
Exercise guidelines for people with diabetes, common glucose trends during exercise, glucose management strategies during and after exercise, and at-home exercise and lifestyle apps that can help you stay healthy
Did you know that a fear of low blood sugar levels (also called hypoglycemia) following exercise is the most common reason people with diabetes have a hard time meeting recommended exercise guidelines? Stanford researcher Dr. Dessi Zaharieva recently presented “Diabetes & Exercise in the Time of COVID-19” through Stanford’s renowned Project Echo Diabetes series. She discussed exercise guidelines, common glucose trends observed during physical activity, and ways to be active at home.
Current guidelines state that people with diabetes should exercise in two ways. First, you should be physically active for at least 30 minutes each day (or 2.5 hours each week) with no more than two days in a row without activity, and you should do muscle-strengthening activities (for example, exercises with free weights or resistance bands) two to three times per week, if your health allows it. For children and adolescents with diabetes, the recommendation for activity is double, at 60 minutes or more each day and the same for muscle-strengthening activities.
Unfortunately, the majority of people with diabetes are not meeting these importance exercise goals:
-
More than half of people with type 1 diabetes are inactive.
-
Fewer than one out of five people with type 1 diabetes exercise more than twice per week.
-
About four out of five people with type 2 diabetes do not meet these physical activity recommendations.
For comparison, about half of US adults met physical activity guidelines for low-intensity exercise in 2018, while fewer than one in four adults achieved both recommendations for low-intensity exercise and muscle-strengthening activity.
Dr. Zaharieva, who lives with diabetes herself, said that without careful monitoring and insulin adjustments, exercise that is characterized by short bursts of energy (called anaerobic or high intensity exercise, such as heavy weightlifting) makes glucose go up, while longer duration but low to moderate intensity exercise (called aerobic exercise, like biking or running) can make blood sugars go down. Activities that combine short bursts and longer low to moderate intensity activity (such as playing soccer with friends) do not cause as much variability in a person’s glucose levels.
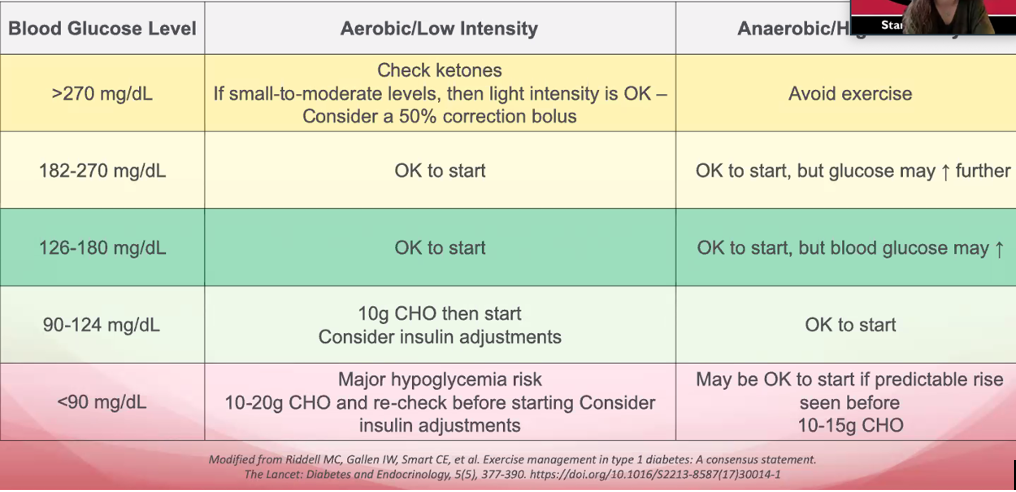
Adjust your exercise plan based on your glucose levels
Knowing how to manage your glucose levels will help you better avoid hypoglycemia after exercise. Dr. Zaharieva focused her recommendations on people with type 1 diabetes or people with type 2 diabetes who use insulin. No matter how active you are, all people with diabetes should consider their goals when planning for a workout. Glucose management strategies may differ if your goal is to “stay in shape,” compete at a high level, lose weight, or train for a long-distance race. In other words, the type, intensity, and duration of exercise will determine how to prepare.
Glucose levels at the start of exercise should be individualized for each person with diabetes – make sure you ask your healthcare professional what numbers may be best for you. In her experience, Dr. Zaharieva finds that exercising with insulin on board (insulin that’s still active in the body from the previous bolus) can be challenging, especially since insulin absorption increases during activity. She recommends exercising in a fasting state and in the morning when blood glucose levels are most stable. Other diabetes care professionals suggest waiting more than 90 minutes after a bolus before exercising, or taking less bolus if you won’t wait a full 90 minutes – however, every person is different. Work with your care team to come up with an exercise plan that works for you and helps you avoid hypoglycemia.
Here are Dr. Zaharieva’s suggested guidelines for exercise:
-
Starting the activity when glucose levels are between 90-270 mg/dL is okay, but it’s important to know yourself and make the necessary adjustments on the low end (by consuming 10 grams of carbohydrates) or on the high end if blood glucose increases. You may find it harder to exercise with high glucose levels.
-
When glucose is below 90 mg/dL there is a major risk of hypoglycemia when doing aerobic (low intensity) exercise. You should consume 10-20 grams of carbohydrates and re-check your glucose before starting the low intensity activity.
-
Starting anaerobic (high intensity) activity when glucose is below 90 mg/dL may be okay if your glucose levels are trending up and you’ve consumed carbohydrates.
-
If your glucose is above 270 mg/dL, avoid intense exercise. Light activity is okay if ketone levels are low. Any correction bolus can cause hypoglycemia (during or after the workout), but you may still consider taking a 25-100% correction bolus knowing that a 1-unit bolus might lower glucose like a 2 or 4-unit bolus. The reduction will depend on the intensity of the workout, insulin sensitivity, and what will be eaten after exercise. Eating a mix of high-fiber carbs, protein, and fat after exercise can also help prevent going low after working out. Read Adam Brown’s “Get in the Zone: My Tips For Avoiding Hypoglycemia During Exercise” for more.
Looking for home workout ideas?
While current exercise options may be limited due to COVID-19, there are plenty of ways that you can stay active at home. For example, walking, doing yoga, running, or biking are great options. You can also think about using soup cans, water bottles, and backpacks as weight substitutes to help you meet the strength training recommendations. If you prefer more structure, there are many free apps and videos available to help you stay on track with your physical activity goals. Here are some of Dr. Zaharieva’s suggestions:
-
Free YouTube exercise channels: Core Power Yoga, Tara Stiles Yoga, Yoga with Adriene, Yoga with Kassandra, Fitness Blender, Body Project, The Body Coach TV, PopSugar Fitness,
-
Free exercise apps: Nike Training Club, Nike Run Club, ToneitUp, FitOn, 7 Minute Workout, Glucose Zone
-
Diabetes lifestyle with exercise apps: T1Exercise, DiaBits, Glucose Buddy, One Drop, Bant, MySugr, Glucose Zone
-
Exercise videos for kids: Cosmic Kids Yoga, Pancake Manor, Go Noodle
-
Exercise for limited mobility and beginners: C25K, Body Project, Kaiser Permanente Thrive
Next week, get ready to hear from Dr. Fran Kaufman on the newest guidelines for exercise for people with type 1 diabetes using continuous glucose monitoring (CGM). She’ll also include key points for people with diabetes to consider before, during, and after exercise. For more on exercise and diabetes, check out diaTribe’s “Exercising Well with Diabetes Using Automated Insulin Delivery,” “The Most Underrated Diabetes Exercise Strategy,” or “Get in the Zone: My Tips for Avoiding Hypoglycemia During Exercise.”







