Treating Hypos: One-Size Does NOT Fit All!

By Gary Scheiner MS, CDE
Imagine if there were only one car on the market. Or one type of breakfast cereal. Or (heaven forbid!) one type of insulin pump. Would you feel a little bit cheated? You should. INDIVIDUALIZATION is where it’s at: customizing whatever it is to best meet your particular needs.
In the diabetes field, healthcare providers and product marketers have been trying for years to stuff a one-size-fits-all approach down our throats when it comes to treating hypoglycemia, using 15 as the magic number. It doesn’t matter who you are, what you’re doing, or how low you are. Fifteen grams of carbohydrate is the magical elixir.
For those of us dealing with hypoglycemia on a regular basis, we understand that this is just plain wrong. Every person is unique, and every situation has its own unique characteristics. And we’re not talking about something superficial here like the body side moldings on a car. We’re talking about dealing with a true medical emergency. Undertreatment of hypoglycemia can result in a seizure, loss of consciousness, or much worse. Overtreatment can produce significantly high blood sugar levels for many hours.
In preparing to treat hypoglycemia (and this is something you should think about now, not when you’re low and can’t think too clearly), consider the following:
1. Body Size
The bigger you are, the more carbohydrates it takes to raise the blood sugar. This is because bigger people have more blood volume into which the glucose will dissolve. Every gram of carbohydrate will raise a small child’s blood sugar much more than that of a fully-grown adult. The chart below summarizes the amount that each gram of carbohydrate could be expected to raise a person’s blood sugar based on their weight:
|
Weight in Pounds (kg) |
One gram of carbohydrate raises blood glucose by… |
|
<60 (>28) |
6-10 mg/dl (.33-.55 mmol/l) |
|
60-100 (29-47) |
5 (.28) |
|
101-160 (48-76) |
4 (.22) |
|
161-220 (77-105) |
3 (.17) |
|
>220 (>105) |
1-2 (.05-.11) |
2. How Low You Are
The lower your blood sugar, the more carbohydrates you will need to get back up to normal. The table below provides a guide based on body size with a goal of raising the blood sugar to approximately 120 mg/dl (6.6 mmol/l). Another way to determine the amount needed for you specifically is with this formula: (Target BG – Current BG) / BG rise per gram of carbohydrate.
For example, if your target is 100 mg/dl, your current BG is 60 mg/dl and each gram of carbohydrate raises you 4 mg/dl, then you need (100-60)/4, or 10g of carbohydrate.
|
Blood Sugar (mg/dl) (mmol/l) |
60s (3.3-3.9) |
50s (2.8-3.2) |
40s (2.2-2.7) |
30s (1.7-2.1) |
20s (1.1-1.6) |
|
Weight: <60 lbs (28 kg) |
9 g |
11 g |
13 g |
15 g |
17 g |
|
60-100 lbs (29-47 kg) |
11 g |
13 g |
15 g |
17 g |
19 g |
|
101-160 lbs (48-76 kg) |
14 g |
16 g |
19 g |
21 g |
24 g |
|
161-220 lbs (77-105 kg) |
18 g |
22 g |
25 g |
28 g |
32 g |
|
>220 lbs (>105 kg) |
28 g |
33 g |
38 g |
43 g |
48 g |
Editor's Note: These numbers should be used as a general guide, since the responses to hypoglycemia can vary based on many factors (e.g., amount of exercise, general level of carbohydrates in the diet, insulin resistance, etc). Unfortunately, it's difficult to study this in a very rigorous fashion and come up with evidence-based guidelines. As a result, we recommend that patients use a mix of these general principles and their own personal experience. If you have not ever done so, try a personal test of how many carbohydrates it takes to raise your blood sugar. Glucose tabs work well for this, since they are typically either four or five grams of carbohydrate each.
3. The Rate of Change
This is easily seen on a continuous glucose monitor. If your blood sugar is low and still dropping quickly, you will need more carbohydrates than the “standard” amount. If your blood sugar is low and leveling off, the standard amount should work fine.

Figure 1. BG low and accelerating downward – consume extra carbohydrates 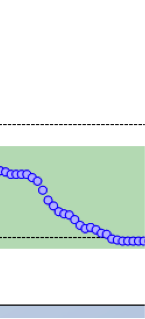
Figure 2. BG low but leveling off – consume “standard” amount of carbohydrates
4. The Sitchy-Ation
We all know that there are a million different variables when it comes to blood sugar management. As I often say, if it were simple, everyone would want it. A few other variables to consider when treating low blood sugar:
- Insulin-On-Board (IOB) – The more rapid-acting insulin you still have working in your body when a low occurs, the more carbohydrates it will take to treat the low. For lows that occur within a couple of hours of a mealtime bolus, extra carbohydrates will probably be needed. For lows that occur more than four hours after administering rapid-acting insulin, the standard treatment should work fine.
- Muscle Activity – If you plan to exercise soon after treating the low, or if you are coming off a bout of intense exercise, extra carbohydrates will be needed. Your muscles will be gobbling up glucose to replenish their energy (glycogen) stores, and that glucose will be drawn right out of the bloodstream.
- Food-On-Board – In the past couple of hours, if you had a meal or snack that consisted of mostly low-glycemic-index foods (such as legumes, dairy products, pasta, salad veggies, or had a great deal of fat along with the carbohydrates), there is a very good chance that some of the meal is still digesting. That doesn’t mean that you should ignore the low blood sugar, but the treatment can be less aggressive than the usual amount.
So forget the “rule of 15”. Unless, of course, you weigh 180 lbs (86 kg), your blood sugar is 65 mg/dl (3.6 mmol/l), your target is 110 mg/dl (6.1 mmol/l), you aren’t still dropping rapidly, you didn’t just exercise, you have no insulin on board, and you haven’t eaten for quite a while. Then it should work to a “T”.
Editor’s note: Gary Scheiner MS, CDE is Owner and Clinical Director of Integrated Diabetes Services (www.integrateddiabetes.com), a consulting practice located near Philadelphia for people with diabetes who utilize intensive insulin therapy. He is the author of several books, including Think Like A Pancreas: A Practical Guide to Managing Diabetes With Insulin. He and his team of Certified Diabetes Educators work with children and adults throughout the world via phone and the internet. Gary has had Type-1 diabetes for 27 years and gone through a small mountain of DexTabs in that time. He can be reached at gary@integrateddiabetes.com.







