Targeting a Cure: A Resource for Type 1 Diabetes Cure Research
On May 1, the American Diabetes Association (ADA) is publishing an updated edition of our book, Targeting a Cure For Type 1 Diabetes: How Long Will We Have to Wait? The eBook is now available for purchase and download in the ADA store at ShopDiabetes.org. The book can be found at this address: http://www.shopdiabetes.org/1419-Targeting-a-Cure-for-Type-1-Diabetes-How-Long-Will-We-Have-to-Wait-ePub.aspx. We hope this will give Targeting A Cure the opportunity to reach a larger audience, and so we have decided to update our original preview of the book from diaTribe #34 in anticipation of the rerelease. We have revised the original article where appropriate to reflect areas in which the research has evolved since the book’s original 2011 publication. Below, we present short excerpts from Dr. Robert Ratner’s foreword and Dr. Aaron Kowalski’s introduction. They are both experts in the field of diabetes research, and we are honored to begin our book with their words of wisdom.
Excerpt from Dr. Robert Ratner’s Foreword
“Targeting a Cure for Type 1 Diabetes by Lisa Rotenstein, Kelly Close, and their colleagues takes on the demanding task of chronicling the status of the various approaches undertaken to achieve a long-sought-after cure. With a perspective of critical optimism, this book describes the arduous research journey that has been traveled in the pursuit of a cure, as well as the minor successes and failures encountered along the way. This book also reminds us that small steps in understanding immunology, beta-cell biology, glucose sensing, and insulin delivery are what provide people like Jim and Sara [friends of Dr. Ratner with type 1 diabetes who have inspired him to work in the field of diabetes] the means of improving their diabetes self-management today while they await the grail of a cure. People with diabetes and their caregivers (including physicians and researchers) should read this book to become informed consumers and providers and to generate the next great and innovative approach to turning that vital corner to cure type 1 diabetes.”
- Dr. Robert E. Ratner
Chief Scientific and Medical Officer, American Diabetes Association
Excerpt from Dr. Aaron Kowalski’s Introduction
“When I think back to 1977, the year my brother was diagnosed, the world was a much different place for people with diabetes. We did not have glucose testing or insulin pumps. Complications were much more prevalent. And the prognosis for a person with type 1 diabetes was frightening. Although we haven’t seen the silver-bullet cure that we have been hoping for, we’ve come a long way. Treatments have advanced significantly, and we are on the cusp of the first artificial pancreas systems. We are also moving very quickly toward biological approaches that will ultimately, one day, allow us to finally walk away from diabetes and prevent our next generation from developing this terrible disease. The future is bright. This book details some of the very promising research that will help us get there. I commend Kelly and the diaTribe team for providing a thorough and understandable view of the state of diabetes research. These are exciting and hopeful times.”
- Dr. Aaron Kowalski
Vice President, Treatment Therapies, JDRF
The following originally appeared as part of learning curve in diaTribe #34. It has been updated to reflect the last two years of work on Targeting a Cure.
Introduction
Since we founded diaTribe in 2006, its focus has always been on providing helpful, practical information to people with diabetes. Our book, Targeting a Cure, aims to go beyond that focus by providing a detailed update on progress toward curing this disease. We hope that you will enjoy learning from it whether you are a person living with type 1 diabetes, a parent or caregiver, a researcher or clinician, or anyone else looking for clear information on an issue that inspires strong opinions and stirring hopes. In writing this book, we have assumed that our readers are interested in details but not that they have deep experience in science or medicine. Though no one knows exactly when a cure will come or what it will look like, we hope that this book will give you a better idea of the possibilities and the promises. We are not blind optimists. We know the hurdles are high. But we also know that the gains made have been substantial, and we believe that a cure will arrive in our children’s lifetimes.
Where Are We Today?
The discovery of insulin in 1922 was one of modern medicine’s greatest breakthroughs and has saved millions of lives. With insulin’s discovery, people with diabetes could hope to live long, productive lives as long as they continued to receive injections of this "miracle" drug. Today, nearly 90 years later, insulin remains the most important drug for people with type 1 diabetes and many with type 2 diabetes, but as the t-shirt says – “Insulin is not a cure.”
Some inroads into the search for a cure have been made in recent years. Our understanding of what causes type 1 diabetes has improved. We have successfully reversed diabetes in some animal models of the disease. We have devised methods to keep transplanted islets alive for longer periods of time. Blood glucose meters, insulin pumps, continuous glucose monitors, Symlin, and other therapies and technologies have enabled better daily management of glucose levels. These advances could eventually lead to preventing, reversing, or overcoming diabetes. But for now, the cure for human type 1 diabetes remains painfully elusive. In Targeting a Cure for Type 1 Diabetes: How Long Will We Have to Wait? we present what we believe are the four most promising categories of therapies that target a cure: immune therapeutics, islet transplantation, regeneration of beta cells, and the artificial pancreas. While all have the same goal, each has its unique advantages and disadvantages, which are introduced below.
What Happens in Type 1 Diabetes
To understand what a treatment would need to do to "cure" type 1 diabetes, we must first understand the changes that occur in the body that lead to this condition. Type 1 diabetes is caused by the destruction of beta cells, cells housed in a structure within the pancreas called islets that are responsible for producing insulin. This drastically reduces the production of insulin.
As many readers will know, insulin is a hormone that allows glucose produced from the carbohydrates we eat to enter the cells of our body that use glucose for nutrition. Healthy beta cells secrete enough insulin to admit the right amount of glucose into cells, but that process breaks down in people with type 1 diabetes because of insulin deficiency.
In people with type 1 diabetes, the immune system destroys the beta cells. The immune system is normally charged with protecting us from bacteria and viruses, but it is thought to destroy beta cells in type 1 diabetes because those cells have been misidentified as “foreign” invaders. Why the immune system misidentifies the beta cells is not yet known but is an active area of research. The theory is that some kind of environmental trigger (a toxin or infection) may inappropriately initiate an immune response in certain genetically susceptible people.
What Does “Targeting a Cure" Mean?
To "cure" type 1 diabetes, a therapy would either have to replace the beta cells that have been destroyed and prevent further beta cell loss, or closely mimic the normal insulin-producing function of beta cells in a way that does not require constant management.
Another way to think of a "cure" is that it would either prevent diabetes from ever happening, halt it in its very early stages, replace lost beta cells, or make up for lost beta cell function without placing additional burdens on the person. A treatment that prevents the development of type 1 diabetes will likely be developed first among the cure therapies (excluding the artificial pancreas; its timeline is discussed below). In addition, a therapeutic cure might not be just one treatment, but could be a combination of several.
Four approaches known as immune therapeutics, islet transplantation, regeneration of beta cells, and the artificial pancreas could potentially achieve these goals. Figure 1 illustrates how each of these approaches may be used to “cure” type 1 diabetes at different stages of the disease.
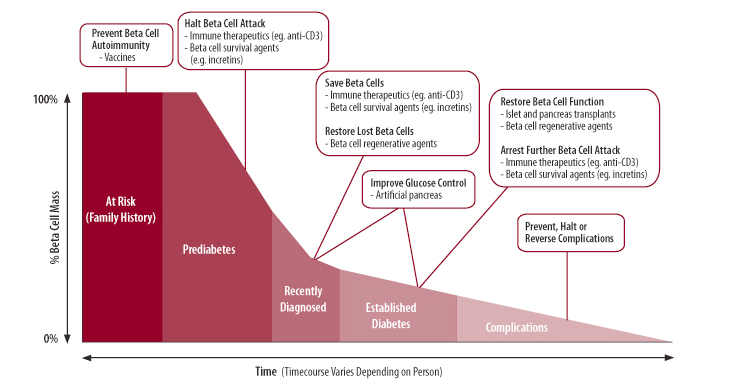
Figure 1. Cure-targeted strategies and therapies for type 1 diabetes broken down by stage of disease. (Adapted from JDRF).
1. Immune Therapeutics
The goal of immune therapeutics is to modify or modulate the immune system in a way that prevents the destruction of beta cells. This approach addresses diabetes at a cellular level, attempting to “cure” the root cause of the disease: the immune system’s components are not functioning the way they should. Several approaches to immune therapy are being developed. These include diabetes vaccines as well as drugs that target specific components of the immune response through a variety of methods, including stopping T cell activation and stem cell therapy. The aim of these therapies is to shut down ongoing beta cell destruction and reinitiate the normal mechanisms that prevent the immune system from destroying healthy parts of the body.
Both of these approaches are discussed in detail in the full report, which surveys several specific therapies and presents much of the current state of basic research and clinical trials. Unfortunately, recent developments in immune therapy have not been encouraging as several recent trials have failed to show adequate efficacy, both for vaccines and for immune modulating drugs. Nevertheless, research in this field continues and several clinical trials are still ongoing.
2. Islet Transplantation
Islets, found in the pancreas, contain a number of different cells – most notably beta cells – that produce blood glucose-regulating hormones. Islet transplantation replenishes lost beta cells through an infusion of islets from another source, which using today’s technology involves islets from a deceased donor. These donor islets are not available in large numbers, substantially restricting the number of transplants that can be performed each year.
Islet transplantation is a potential cure in that the transplanted "new" islets will work in place of destroyed ones. In fact, estimates suggest that over two-thirds of people who receive islet transplantations no longer require insulin injections one-year after the procedure. The procedure works well and lowers insulin dose requirements or removes the need for injectable insulin entirely. Unfortunately, this treatment is not long lasting, and five years after transplantation, only 10% of people remain independent of insulin therapy.
The biggest risk of islet transplantation is the accompanying immune suppressive therapy, which is necessary to prevent rejection of the transplanted islets just as it is necessary after transplantation of any organ from an unrelated donor. Immune suppressive drugs have many side effects, including damage to the kidneys, and an increased risk of infection and developing particular types of cancer.
Many companies and academic researchers are trying to develop new methods to generate beta cells for transplant, and they are trying to induce the acceptance of transplanted beta cells without the need for immune suppression. These areas of research are discussed in detail in the book, as it examines developing beta cells from human stem cells, harvesting islets from pigs, and producing mechanical barriers to prevent contact between the transplanted cells and the immune system.
3. Beta Cell Regeneration and Survival Therapies
In light of the challenges of islet transplantation, the discovery of ways to stimulate new beta cells to grow in the pancreas, and ways to protect the cells’ health and survival, would represent a major leap forward.
If successfully developed, drugs that stimulate beta cell regeneration could be used for any type 1 diabetes patient to restore beta cells and stop insulin therapy. Such drugs could also halt the progression of type 1 diabetes in the early stages of the disease, by (ideally) stimulating a significant increase in beta cell numbers.
Animal research has provided scientists with useful targets for regeneration therapies, which are discussed in the book. In addition, considerable attention has been turned to the use of incretins (a group of drugs that includes two classes for type 2 diabetes). Basic research in animals indicates that incretins can help beta cells survive longer and regenerate more readily, giving them the potential to ameliorate type 1 diabetes.
4. The Artificial Pancreas
The artificial pancreas (AP), though not a cure in the traditional sense, is a promising technology in our view. The AP is an automated device that tries to reproduce the function of a normal pancreas by delivering the right amount of insulin (and maybe other hormones) to maintain normal glucose control. In the AP, a continuous glucose monitor (CGM), an insulin pump, and a control algorithm work together to mimic the function of a pancreas. A truly “closed loop” AP would require no intervention from the patient, while an “open loop” would still require some intervention (e.g., during meals and exercise). We see the AP as a bridge to a true “cure” for diabetes, though one with significant potential to improve glucose control (particularly for reducing hypoglycemia), reduce the burden of diabetes, and improve patients’ quality of life.
The artificial pancreas has made tremendous advances in recent years. For the first time, large scale trials are being done outside of hospitals and in patients’ homes – encouragingly, these are happening all over the world, including the United States. Studies are also using highly portable, wireless systems for the first time, meaning that patients are no longer wired to bedside laptops to automatically control their blood glucose. To challenge these systems, trials are introducing heavier meals and more intense exercise routines. The systems are also using new approaches to speed insulin action and even employing other hormones. Industry is investing as well – companies like Medtronic, Tandem, and Animas have AP systems in development (with Tandem and Animas partnering with Dexcom for the CGM component of the AP). Their plans are to bring the AP to market in the coming years. In its final guidance document, the FDA has laid out a regulatory path to bring the artificial pancreas to market, incorporating almost all of the recommendations that the JDRF requested in the months leading up to its release. As noted in this issue’s conference pearls, we’re also glad to see open dialogue between the FDA and researchers developing the AP.
One of the biggest problems facing the development and use of an AP is that exercise, meals, stress, sleep, and other factors can all influence blood glucose, and these can be very difficult for current technology to handle. Fortunately, in the coming years, these problems can be addressed with increasingly sophisticated algorithms, more accurate CGMs, faster insulin, and the use of other hormones.
Targeting a Cure provides much more background on the AP, including recent developments and trials and future areas of research.
Conclusion
The progress that researchers have made is exciting, and we believe ultimately hopeful. Though a cure will not be here tomorrow, we believe that each of the broad categories discussed in this report has promise, and that one or several will one day be an option for the cure.
If you are interested in learning more about these areas, together with our perspective on their chances for success and when they will come to fruition, please download at the ADA’s website our eBook Targeting A Cure for Type 1 Diabetes: How Long Will We Have to Wait?







