New Debates on an Old Standard: The A1c Test
by nick wilkie
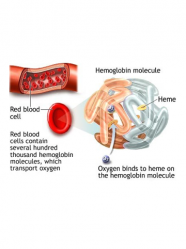
One of the more controversial issues in diabetes today is the use of the A1c test to diagnose diabetes instead of the current standards of fasting plasma glucose (FPG – measures blood glucose after a 12-14 hour fast) or oral glucose tolerance tests (OGTT – blood glucose is measured after the patient consumes a standardized amount of glucose). We gave an in depth explanation of the A1c test in an earlier Learning Curve. In short, the A1c test allows physicians to approximate a person’s average blood glucose over the past three months. So, when your blood sugar is consistently high, it is reflected by a higher than normal A1c. The test is simpler for patients (no fasting or ingestion of glucose is necessary), and its results are more consistent than either FPG or OGTT. There has been a great deal of debate on how to interpret and express A1c results, however. In the December issue of the scientific journal Diabetes Care, Dr. Zachary Bloomgarden, summed up the many talks that were given on the A1c test at the 2009 American Diabetes Association (ADA) Scientific Sessions (for our coverage of this meeting, see Conference Pearls from diaTribe #16).
Possibly one of the most highly talked about sessions at the 2009 ADA Scientific Sessions was given by Dr. David Nathan, a member of the authoring committee for this document. In his talk, he defended the use of A1c for both diagnosis and long-term monitoring of diabetes. His main argument was that A1c better indicates a person’s long-term exposure to high blood glucose than either fasting glucose or glucose tolerance. Potentially most importantly, A1c levels do not vary drastically from day to day in a person. FPG and OGTT, on the other hand, are sensitive to factors such as stress and forgetting to fast. Because of this, doctors can be confident that a patient’s A1c has not been influenced by arbitrary short-term factors.
Dr. Nathan made the case that A1c has not been included as a standard test because the early laboratory methods for measuring it were inaccurate. An expert committee found in 2003 that the A1c test was not yet accurate enough for clinical diagnosis, but Dr. Nathan argued that current methodology allows for much more consistent and accurate measurements than what was available in 2003.
Dr. Bloomgarden, however, questioned the relationship between blood sugar and A1c. In particular, he noted that individual differences can alter how A1c correlates with average blood sugar. Factors that can interfere with this relationship include certain genetic variations, race, age, and certain disease states such as kidney failure or anemia (iron deficiency). Because of this, Dr. Bloomgarden argued that it would be inappropriate to use A1c as a standard for the entire population, especially when people with diabetes have high rates of anemia and kidney failure. He also cited data from a large US census showing that many people that would be diagnosed with diabetes using FPG had A1cs lower than 6.5%, which could lower the rate of legitimate diabetes diagnoses.
Since A1c can be used to approximate a person’s average glucose level, some have suggested that A1c be expressed in terms of an average blood glucose level rather than as a percentage. Using a mathematical formula, the A1c percentage can be converted to an estimated average blood glucose level (for the past three months), abbreviated to eAG. (To calculate your eAG from your A1c, you can use the chart or the formula in Figure 1.) Dr. Bloomgarden highlighted a talk given by Dr. Eric Kilpatrick from Hull in the UK on the clinical use of eAG. Dr. Kilpatrick worried that using this measure would be confusing to patients, since the values may be different from what they see with their home blood glucose measurements. This could lead them to question whether to trust the results from their blood glucose meter or their A1c. He argued that because of this and worries about the accuracy of the A1c-blood glucose relationship, that eAG was premature for clinical use. Dr. Nathan disagreed, however, noting that expressing A1c as average glucose would allow all diabetes measurements and glycemic targets to be expressed with the same units.
Dr. Bloomgarden concluded that, although A1c is an appealing tool for monitoring long-term glycemia, it has a fundamental problem in that its relationship with blood sugar can be different between individuals. Thus, he believes that it is too early to use A1c as a sole measure for diagnosing diabetes, and that interpretations such as eAG should be used with caution.
Figure 1: A1c vs. Estimated Average Blood Glucose
| A1c | eAG (Average Blood Glucose) |
| 5.00% | 97 mg/dL |
| 5.50% | 111 mg/dL |
| 6.00% | 126 mg/dL |
| 6.50% | 140 mg/dL |
| 7.00% | 154 mg/dL |
| 7.50% | 169 mg/dL |
| 8.00% | 183 mg/dL |
| 8.50% | 197 mg/dL |
| 9.00% | 212 mg/dL |
| 9.50% | 226 mg/dL |
| 10.00% | 240 mg/dL |
| 10.50% | 255 mg/dL |
| 11.00% | 269 mg/dL |
| 11.50% | 283 mg/dL |
| 12.00% | 298 mg/dL |
Formula: eAG (in mg/dL) = (A1c * 28.7) - 48.7







