Intermittent Fasting: Stabilizing My Morning Blood Sugars
 By Justine Szafran
By Justine Szafran
Justine shares her experience using intermittent fasting to keep her morning blood sugars in range and to feel better all day long
Intermittent fasting and time-restricted feeding (IF/TRF) have been receiving a lot of praise, and for good reason. These approaches to meal timing create blocs for either consuming food or fasting during certain hours of the day. One common approach to IF/TRF is to only eat within the same eight-hour window. Outside of that time you can have water, unsweetened tea, or coffee. This lets your body reap the benefits of extended periods of fasting. As a person with type 1 diabetes though, I was unsure how IF/TRF might affect my blood sugar management and my ability to stay in range throughout the day.
When the body is in a “fasting” state, it operates differently than when we are in a “feeding” state. When fasting, you use energy that is already stored in your body rather than taking it from your most recent meal. Time-restricted feeding consists of scheduling time for food intake, while intermittent fasting also involves restricting the number of calories you consume. However, if you have type 1 diabetes, it is important to remember that ketone levels may rise during the time that you are not eating. This may be a challenge if you are not getting enough basal insulin and depend on meal-time insulin to avoid high levels of ketones. The good news is that you can measure your own ketone levels. It is also extremely important to monitor blood glucose levels – hypoglycemia is a risk of fasting.
There are powerful benefits to adopting a scheduled eating window for both your body and brain. TRF and IF have been shown to help with things like aging, metabolism, focus, and insulin sensitivity, but I didn’t know how this would affect my diabetes. To read more about the science behind IF/TRF, see the New England Journal of Medicine’s review on intermittent fasting and the American Heart Association’s review on how meal timing can affect heart health.
As people with diabetes know, morning blood sugars are especially challenging. I was curious to see how TRF could affect not only my blood sugar levels in the morning but also how it might affect how I felt throughout the day. I was worried that without eating first thing in the morning, my blood sugar might drop too far below my ideal range, or I might be unreasonably hungry and irritable. I had been told that a low-carb or complex-carb breakfast first thing in the morning was important for setting my day up for success and maintaining optimal blood sugars. However, after years of frustrating morning highs that could last for multiple hours, leaving me tired, groggy, and irritable, I decided to give time-restricted feeding a try.
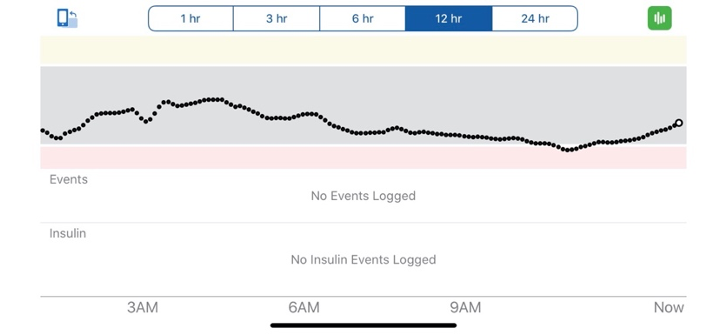
After just a few days of experimenting with eight hours per day of TRF, I knew I’d found a really exciting tool for managing my diabetes more effectively. Now, depending on when I first eat, I’ll stop eating around 7 or 8 PM (you can see my overnight blood sugar levels on the 12-hour graph). This allows for an eight hour “eating window” and a 16 hour “fasting window” – a common time ratio for time-restricted feeding. Getting used to the new eating schedule wasn’t immediately easy, but I found that waking up with just some coffee was enjoyable and the adjustment wasn’t too uncomfortable. I still drink coffee in the morning because it has always been part of my routine and helps me to wake up and be productive. While there aren’t carbohydrates in coffee, the caffeine content raises my blood sugar, so depending on where my blood sugar is, I might give myself half a unit to a unit of insulin to counteract the effects of the caffeine.
In the morning, there are higher levels of hormones that are active in our bodies, and as we wake up our blood sugar naturally rises. Before TRF, even when I was waking up in range, trying to have perfect breakfast dosing and successfully managing my morning highs were significant challenges. I believe I was also experiencing a bit of insulin resistance early in the morning due to the increased hormones. It seemed like regardless of how much insulin I gave myself or how many carbs I ate in the morning (I experimented with only having low-carb breakfasts and longer lead times for my breakfast dose), I found that my blood sugar consistently rose much higher than I wanted it to. I also didn’t want to take a lot of insulin first thing in the morning because it meant I would spike early and crash later on. Too often, all the insulin I used to lower the extreme high from breakfast would catch up with me, and I would end up too low by late morning. Unless I wake up low, I now typically postpone breakfast until my 16-hour fast is up.
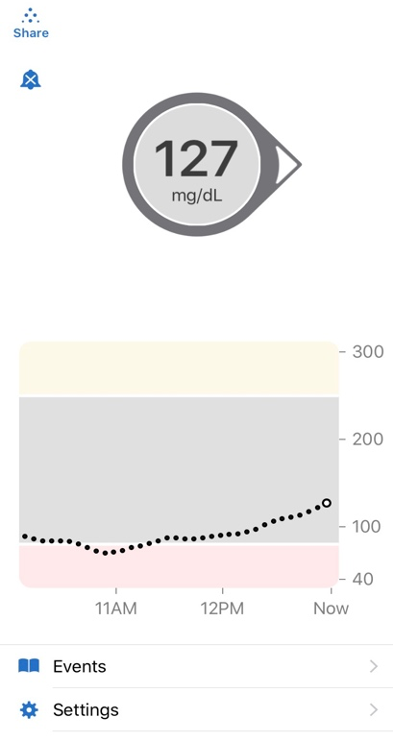
One of the first things I noticed when I started TRF was how much better I felt in the beginning of my day. I was able to be a lot more productive early on and feel my absolute best from the very start of my day. Instead of experiencing grogginess and feeling ill from prolonged high blood sugar levels, I could keep my blood sugar well within my ideal range at least until it was time to eat. When it was finally time to have breakfast, I also discovered that I was noticeably more sensitive to insulin. This meant that I needed less insulin to cover the carbs than I used to. I found that whole grain toast with avocado worked well for breaking my fast. The fat from the avocado kept me feeling full for a while, and the carbs in the bread gave me a boost of energy without sending my blood sugar skyrocketing. Other meals that work for me are overnight oats with berries or, if I break my fast later in the morning, I’ll have a salad with chickpeas. On the graph you can see my blood glucose increase after I broke my fast.
Before TRF, I used to always exercise in the morning. Now, I have found it helpful to shift my workout routine to later in the afternoon or evening after I’ve broken the fast and have had a snack, because that is when I feel the most ready and well-fueled to do so. Because of my higher insulin sensitivity too, I’ll decrease my basal rate a little or suspend the insulin before and during my workout. Staying well-hydrated is also important when using time-restricted feeding and helps me feel my best during workouts.
I’ve found that by increasing the number of hours I don’t eat – not only while sleeping but also including a few hours before bed and after waking up – I have greater insulin sensitivity throughout the day, I can more easily stay within my target blood sugar range, and I feel dramatically more focused and energized in the morning. It has also helped me ensure that I go to bed with a stable blood sugar level and that I remain within my target range throughout the night. Time-restricted feeding drastically shifted the way I approach my daily life with diabetes and has helped me manage my blood sugar and general well-being more effectively.
It was somewhat challenging to adjust to not eating right away in the morning. While this kind of schedule and lifestyle might not be ideal for everyone, this eating pattern has helped me optimize my health and make life with diabetes as easy as possible; I believe the benefits have been well worth the initial challenges.
For more information about intermittent fasting, read: To Skip or Not to Skip: Does Intermittent Fasting Help People with Diabetes?
Editor's note: time-restricted feeding and intermittent fasting are not for everyone with diabetes. It’s important to discuss this change in diet with your healthcare team before giving it a try; you may need to adjust your insulin or other medications, test your ketones, and take additional precautions. It is also important to be aware that time-restricted feeding and intermittent fasting can lead to unhealthy eating habits, including disordered eating. If you are concerned that you or someone else with diabetes may be experiencing disordered eating, contact the Diabulimia Helpline or We Are Diabetes; the National Eating Disorders Alliance is a resource for anyone with or without diabetes.
.jpg) About Justine
About Justine
Justine loves spending time outdoors and making art. She graduated from Carleton College in 2019, with a double major in Political Science and Studio Art. Justine currently works at Carleton College as an Educational Associate in Studio Art, specializing in drawing, printmaking, and ceramics. She enjoys rock climbing, cycling, teaching kids how to sail, and writing.
Justine has been living with type 1 diabetes for 12 years and is always looking for new ways to make life with type 1 easier to manage.







