How Diabetes Care and Education Specialists Can Help: An Interview with Cleveland Clinic’s Phenomenal Dr. Diana Isaacs
By Timothy Hay
Dr. Diana Isaacs on CGM, “shared” appointments, and identifying “Bright Spots” and “Landmines.” Plus, how to find a Diabetes Care and Education Specialist near you
Dr. Diana Isaacs is a Clinical Pharmacist and Diabetes Care and Education Specialist at the Cleveland Clinic. Her job is to work with people with diabetes on a range of important issues, including medications, technology, and lifestyle changes.
Dr. Isaacs is the coordinator for the Cleveland Clinic’s continuous glucose monitor (CGM) program, which means one of her most important roles is to teach people how to use CGM. She meets with 200 people every month, through individual appointments, classes, phone follow-ups, and virtual visits. She also works with other healthcare providers including nurses, nurse practitioners, dietitians, and physicians.
Dr. Isaacs on CGM, Identifying “Bright Spots” and “Landmines”, and Shared Appointments
“CGM is the jumping-off point to general education about diabetes and health,” she said. For her shared appointments, she uses the white board to write out the participants’ “Bright Spots” and “Landmines.” The classes are usually 4-6 people with all types of diabetes including type 1 and type 2.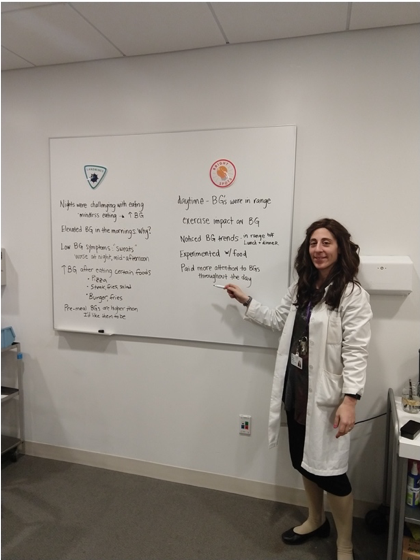
A Bright Spot that came up in one class was a person who learned: “Eggs for breakfast don’t raise my blood sugar as much as oatmeal. I plan to eat more eggs.”
Another person noted a Landmine: “Drinking a whole bottle of pop [soda] to treat my low blood sugar spiked me up way too high.”
The people who attend the shared appointment learn from each other’s CGM data and receive peer support. For example, a person who was nervous to start a new medication agreed to try it after receiving encouragement from others.
In addition to education and adjusting medications, Dr. Isaacs trains people starting on insulin pumps. After initial learning sessions, there are weekly “pump it up” classes that cover different pump topics and can help people make insulin pump adjustments.
Dr. Isaacs said she is also excited about the development of automated insulin delivery (closed-loop) systems, as these innovations could take much of the work out of managing diabetes.
Her Resources
Cleveland Clinic supports people in weight management efforts through shared medical appointments. Dr. Isaacs often refers people to this program with monthly appointments and peer support. These programs are much more than following a diet. They focus on stress, sleep, physical activity, eating patterns, and medications.
The Clinic has a number of its own books and other educational materials that serve as resources for diet and various lifestyles, but Dr. Isaacs said she also frequently turns to diaTribe, including sections of Bright Spots & Landmines: The Diabetes Guide I Wish Someone Had Handed Me by diaTribe Senior Editor Adam Brown during her classes.
“It’s overwhelming when people are first diagnosed,” she said. “There is so much to learn about the routine, food, medications and devices. That’s why we use an interprofessional team approach with the person at the center. Every person is unique and so we have a wide variety of programs to choose from offering individual appointments, shared appointments, and peer support to navigate through all of the new and constantly changing information.
Outside the Classroom
While many insurance plans cover an in-person educational session on CGM use, insurers won’t necessarily cover follow-up meetings with a pharmacist Diabetes Care and Education Specialist – held over the phone, video chat, or in person – to discuss medication adjustments or other aspects of care. That means Dr. Isaacs can’t bill for these follow-ups.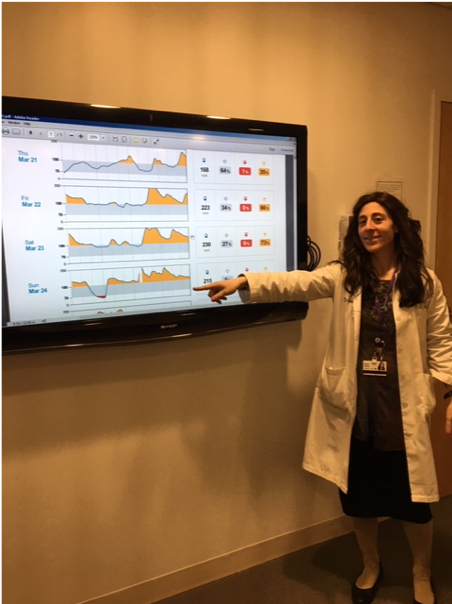
“I’ve been hired to improve health outcomes and meeting that goal means offering certain services for free.” The frequency of visits varies depending on the person’s needs. She typically follows up weekly with pregnant women or other high-risk people. For other people, her visits may be monthly or every other month.
Dr. Isaacs wants people to know that educating is just one aspect of the Diabetes Care and Education Specialist’s role.
“There’s a whole movement now at the American Association of Diabetes Educators (AADE) to change the vision, and remove the perception that we are just educators,” she said.
Diabetes Care and Education Specialists are an integral part of coordinating care, which requires getting to know people and their health habits so they can advise on how to maintain good health. Diabetes Care and Education Specialists also address other related conditions like weight management, blood pressure, cholesterol and emotional health. They also strive to reduce health-system costs by reducing hospitalizations through avoiding severe hypoglycemia and diabetic ketoacidosis (DKA), and reducing other diabetes complications.
According to Dr. Isaacs, “Every person with diabetes should have a diabetes educator. We are here to help.”
How Can I Find a Diabetes Care and Education Specialist?
Use this valuable tool to find a Diabetes Care and Education Specialist near you. In the United States, when working with a diabetes educator accredited by the AADE or ADA, the sessions are covered by Medicare and most private insurance plans. For any insurance coverage of these sessions, you must typically be referred by a healthcare provider.
Under Medicare Part B, up to 10 hours of initial sessions are covered; following the initial training, you may be eligible for 2 hours of training a year. With Medicare coverage, you still pay 20% of the sessions’ cost. Private insurance plans are usually similar to Medicare coverage.







