Weight Loss, Keeping Lost Pounds Off – Is there a Recipe for Success?
By Hope Warshaw
 The American Diabetes Association’s 82nd Scientific Sessions brought together experts across all areas of diabetes care, including for overweight and obesity management. Read about the science and their pearls of wisdom.
The American Diabetes Association’s 82nd Scientific Sessions brought together experts across all areas of diabetes care, including for overweight and obesity management. Read about the science and their pearls of wisdom.
Most people diagnosed with prediabetes or type 2 diabetes have excess weight or obesity. They may also have other conditions at the same time, including abnormal lipid levels, high blood pressure, sleep apnea and more.
Research has shown that losing roughly five to 15 percent of body weight from a starting weight can put prediabetes or early-onset type 2 diabetes into remission, or at least slow the progression of either condition. Remission can also improve the status of related health conditions and lower the doses and number of medications an individual takes.
However, in order to maximize these health benefits, it is crucial to keep as many of those lost pounds off as possible. Speakers at the 82nd ADA Scientific Sessions held in New Orleans tackled this topic, sharing their pearls of wisdom in the session titled, Maximizing Weight Loss Maintenance—Ingredients for the Secret Sauce?
Dr. Hollie Raynor, nutrition professor at the University of Tennessee Knoxville, and a dietitian, psychologist, and researcher, was the first speaker. Raynor spoke on four evidence-based strategies to maximize remission through weight loss.
-
First, get plenty of physical activity. According to the ADA 2022 Standards of Care, this includes four components: 1) aerobic exercise, 2) resistance training, 3) balance and 4) flexibility training as well as decreasing sedentary activity. “Physical activity, while important in weight loss, is even more critical for keeping lost pounds off, requiring some physical activity nearly every day,” said Raynor. “People who successfully integrate physical activity [are those who] identify activities that they can easily and regularly engage in and that they enjoy doing.”
-
Second, self-monitor your progress through tracking of weight, food and physical activity – this is essential for losing weight and keeping it off. Ideally this should be done regularly; however, it can be challenging to self-monitor forever. To ease the burden, Raynor suggests using technology like food and activity apps, or only monitoring during problematic periods of weight gain or diabetes management.
-
Third, set small goals. Behavior change is at the core of successful weight loss maintenance. Setting small goals and resetting goals as needed can help achieve success. Experience success. Evaluate your goals. Repeat. This cycle can build positive experiences and what researchers call sell-efficacy, or the “I can do it” attitude.
-
Finally, reduce caloric intake and develop a personal eating plan. “The ability to reduce the calories one eats is at the crux of any weight loss intervention,” said Raynor. She added that while there is still debate about which type of diet or approach is best, “what’s key is a person’s ability to adhere to their chosen eating plan and integrate it into their lifestyle long term.”
At the end of her presentation, Raynor responded to a question about research on intermittent fasting and time-restricted eating as a strategy to manage weight. Raynor noted that some of these eating patterns have been helpful and others not. A challenge for researchers, Raynor said, is that there are no standard definitions for intermittent fasting or time-restricted eating, which makes it hard to compare studies.
Linda Delahanty, director of nutrition and behavioral research at Massachusetts General Hospital’s Diabetes Center and associate professor of medicine at Harvard Medical School, reiterated Raynor’s message that the focus must be on building skills to enable behavior changes in eating and food choices. She added that when setting goals, problem solving and trial-and-error are key to finding the optimal approach.
“You must identify your why – your overarching purpose for weight loss – and keep this top of mind,” said Delahanty. “Is it not developing type 2 diabetes or being in shape to play with grandchildren?”
 Also, Delahanty shared encouraging data on the impact that weight loss can potentially have for individuals at risk for type 2 diabetes, from her days working on the NIH-funded Diabetes Prevention Program (DPP). Results from the DPP showed that for every 2.2 pounds of weight loss, the risk of developing diabetes was reduced by 16%. In addition, doing 150 minutes of physical activity per week reduced the risk of developing type 2 diabetes by 44%. More weight loss and more physical activity helped people achieve lower glucose levels, improved A1C, lower blood pressure and triglycerides, and reduced dose and number of medications.
Also, Delahanty shared encouraging data on the impact that weight loss can potentially have for individuals at risk for type 2 diabetes, from her days working on the NIH-funded Diabetes Prevention Program (DPP). Results from the DPP showed that for every 2.2 pounds of weight loss, the risk of developing diabetes was reduced by 16%. In addition, doing 150 minutes of physical activity per week reduced the risk of developing type 2 diabetes by 44%. More weight loss and more physical activity helped people achieve lower glucose levels, improved A1C, lower blood pressure and triglycerides, and reduced dose and number of medications.
Delahanty discussed how important it is to recognize that there will be “slips” along the weight loss journey, advocating for, as she put it, “relapse prevention.” This involves finding ways to stay motivated and learning how to manage adversity or situations with a high risk of “slips,” such as eating away from home, special occasions, or stressful situations.
“For the long haul, people must master the skills to balance structure and flexibility and to make the mental mindset shift from black and white, on/off thinking,” Delahanty said. “They don’t have to eat perfectly every day. They need to eat better on more days.”
 As parting advice, Delahanty suggested that people with prediabetes consider enrolling in the clinically proven CDC National Diabetes Prevention Program. She suggested that people with early type 2 diabetes and overweight or obesity seek out the services of a registered dietitian nutritionist or a research-based weight management program.
As parting advice, Delahanty suggested that people with prediabetes consider enrolling in the clinically proven CDC National Diabetes Prevention Program. She suggested that people with early type 2 diabetes and overweight or obesity seek out the services of a registered dietitian nutritionist or a research-based weight management program.
“Find the ingredients that produce your recipe for success,” Delahanty said. “There’s no one way or right way and no one size fits all.”
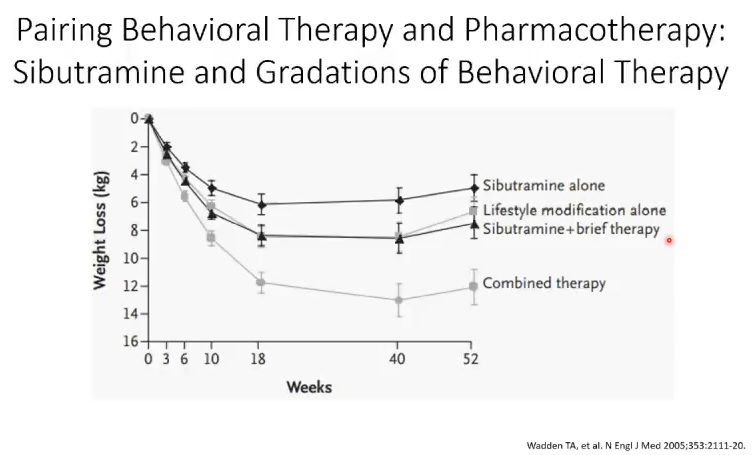
While lifestyle adjustments and a resilient mindset can make a significant impact, many people could also benefit from certain types of medications with dramatic weight-loss properties. Dr. Scott Kahan, director of the National Center for Weight and Wellness and faculty member at George Washington University School of Medicine and Johns Hopkins Bloomberg School of Public Health, discussed how a combination of medications and behavioral adjustments can be most effective in managing weight long-term.
“Sometimes people need the help a medication can offer and a handful of these have been shown to help,” said Kahan. In sharing the research, Kahan showed that adding an effective medication almost always leads to more weight loss and to other improved health outcomes.
The future of weight management medications looks particularly bright now with the newer categories of obesity management and glucose lowering medications that demonstrate weight loss. These medications include SGLT-2 inhibitors, GLP-1 receptor agonists, and tirzepatide (currently approved under the brand name Mounjaro, it is the newest medication in a new drug class known as “dual agonists” or “dual GIP/GLP-1 receptor agonists”).
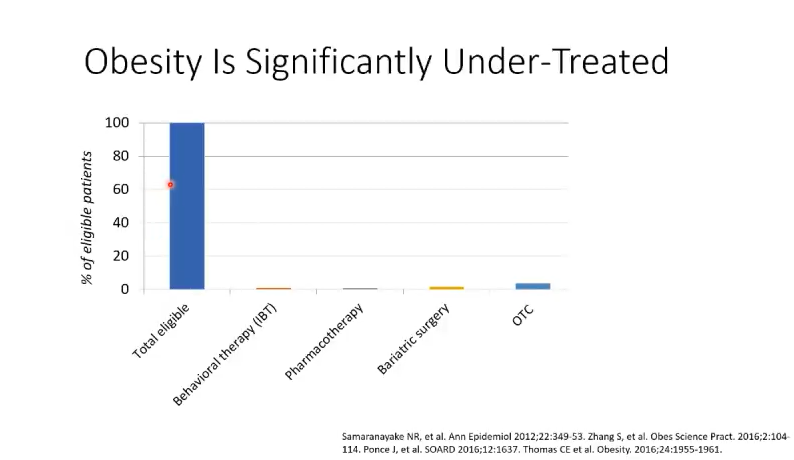
To discuss why more weight loss medication is not used, Kahan presented data from several studies showing that obesity is a significantly under treated disease. Almost no provider is prescribing any of these medications; thus, almost no one with obesity benefits from them. “Obesity is a chronic condition that requires chronic support with continued therapies,” he said.
Kahan recommends sequential management, meaning that people should start with behavioral counseling and then, if needed, add medication. “Perhaps consider introducing medication when a person experiences some weight regain to ‘bend the trend back down,’” he said.
As these three experts discussed throughout this ADA session, there are several different strategies to approach weight management, with different strategies working for different people. All in all, managing excess weight and obesity play a significant role in successful risk reduction and management of prediabetes and type 2 diabetes and related diseases.
Find additional information in the following resources on obesity and diabetes, exercise, nutrition, and more.








