New Intestinal Treatment May Help Type 2 Diabetes Patients Stop Taking Insulin
By Susannah Chen
 Early-stage study results show that a new one-hour intestinal procedure called ReCET may be able to help people with type 2 diabetes improve their blood sugars enough to stop insulin treatment.
Early-stage study results show that a new one-hour intestinal procedure called ReCET may be able to help people with type 2 diabetes improve their blood sugars enough to stop insulin treatment.
A new outpatient intestinal procedure could not only help people with type 2 diabetes manage their blood sugar, but it could also help them get off insulin altogether: That’s the assertion one company, Endogenex, is making based on new results of a study it’s presenting at Digestive Disease Week in Chicago.
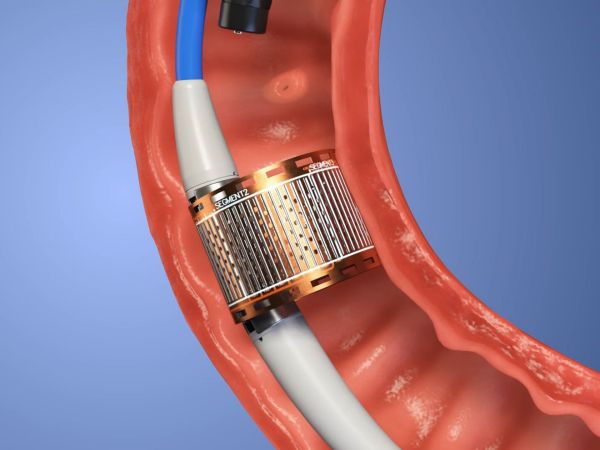
ReCET (re-cellularization via electroporation therapy) is a one-hour procedure developed by Endogenex that delivers electric pulses to regenerate cells in the lining of the duodenum. The duodenum is the first part of the small intestine that helps digest food, absorb water, and relay information between the gut and the brain.
In a study called EMINENT, 14 people with type 2 diabetes between ages 28 and 75 who were all taking long-acting basal insulin successfully underwent ReCET with no serious adverse events. They were then put on a calorie-controlled liquid diet for two weeks, then started on the GLP-1 receptor agonist medication semaglutide (the generic name for diabetes drugs Ozempic and Rybelus and weight loss drug Wegovy) following that, slowly increasing the dose up to 1 mg per week.
In the first study in humans funded by Endogenex, 12 of the 14 participants, or 86 percent, were able to come off insulin treatment at six months and remain off insulin treatment for a year following the ReCET procedure combined with the use of semaglutide.
According to Dr. Jacques Bergman, principal investigator on the study and an Endogenex advisory board member, the company hopes to improve the ReCET procedure so that it can be used on a large scale for many more people with type 2 diabetes. “We expect the ReCET procedure to be further simplified [as research continues].” he said.
This process, also known as duodenal mucosal regeneration (DMR), is similar to Fractyl Health’s Revita DMR procedure. But unlike Fractyl Health’s procedure, which Bergman was also involved in studying, ReCET does not use heat or cold to disrupt the intestinal tissue, which may reduce the chance of complications.
While semaglutide on its own sometimes allows people with type 2 diabetes to stop taking insulin, the ReCET procedure may further improve the chances of not needing insulin.
“In most studies in which patients on long-acting insulin receive a GLP-1 receptor agonist, less than 20% can stop insulin completely,” said Celine Busch, the study’s lead researcher and graduate student working towards her PhD at Amsterdam University Medical Center. “It’s difficult to explain our results based on [only the use of] semaglutide.”
After 12 months of follow-up, study results also showed that A1C improved from 7.2% to 6.6%; fasting glucose levels improved from 158 mg/dL to 119 mg/dL; liver fat percentage was reduced by greater than 50%.
The small study has not yet been published or peer reviewed, but Endogenex plans to confirm the results with a randomized controlled trial in the future.








