Lee Kaplan, MD, PhD Discusses “Bypassing by the Bypass”: A Perspective on Novel Obesity Therapies
By Kelly Close

by sanjay trehan and kelly close
We recently had a fascinating discussion with obesity expert Dr. Lee Kaplan on the future of medical and surgical obesity therapies as well as hot topics in obesity research. An Associate Professor of Medicine at Harvard Medical School, Dr. Kaplan also serves as the Director of the Weight Center at the Massachusetts General Hospital in Boston, widely considered one of the leading obesity clinics in the world. Dr. Kaplan is a leading researcher in gastric bypass surgery and also the Director of the Obesity Research Center at Mass General. We were especially intrigued by his research on the physiological effects of bariatric surgery and his hopes to one day “bypass the bypass” – in other words, to mimic the effects of surgery without the surgical procedure. Dr. Kaplan also provided a useful overview of the specific effects of surgical therapies that lead to resolution of diabetes and/or obesity, as well as his thoughts on the growing acceptance of bariatric surgery – read on.
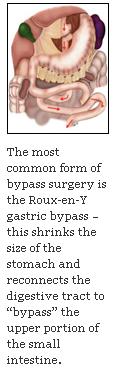
In this interview, Dr. Kaplan shares intriguing insight on the effects and future of weight loss surgery. For more on the gastric bypass procedure – the most common form of bariatric surgery in the United States – see here.
dr. kaplan and his practice
Kelly: Dr. Kaplan, thank you so much for taking the time to speak with us. To start, we would love to learn more about the Weight Center that you run at Massachusetts General Hospital. Could you tell us about the patients that your center admits?
Dr. Kaplan: We see about a thousand new patients a year, with an average body mass index of roughly 50, and of these patients about 25% to 30% eventually undergo surgery. We see patients exclusively by medical referral, and the demand, not surprisingly, is very high. Physicians typically refer the patients who most need our specialized care and, as a result, we have a high percentage who are treated with medications or surgery. Nonetheless, the majority of our patients are treated primarily with counseling and lifestyle therapy.
Kelly: We assume if placed on the waiting list, it takes several months to be able to see someone on your team.
Dr. Kaplan: Yes. Assuming that about 25% of the adults in Massachusetts have obesity, which is lower than the national average, we estimate that more than 50,000 patients who are cared for at Mass General have obesity. At a thousand patients a year, it would take us 45 or 50 years to see them all. So clearly, it doesn’t make sense for us to evaluate or care for every patient with obesity. Just as everyone with heartburn does not require specialized GI care, most people with obesity can be cared for by their primary care provider. We view ourselves as specialists in obesity medicine, and that the best use of our specialized focus is to provide care for patients with obesity that is severe or complicated enough that primary care providers (PCPs) cannot manage optimally. One of the major problems in this area is that many PCPs feel that they cannot adequately manage patients with obesity because we don’t have particularly effective therapies. For the average person with obesity, however, I think that PCPs could be educated to do as good a job as a specialist and that is what should be done. When you get into complicated situations that require complex medical regimens or surgery, then you obviously want patients to have access to a specialized center, and that’s where we come in.
Kelly: How many other specialists are there in the center that you lead and how many patients, in total, would you say have been seen at the Weight Center since it opened 11 years ago?
Dr. Kaplan: There are three other internists, two pediatricians, three dietitians, three psychologists, and four surgeons. We have seen approximately 8,000 patients since the Center opened.
the current and future environment for obesity therapies
Sanjay: There seems to be a variety of available therapies with limited efficacy and several side effects. Could you give us a broad overview of the current environment for obesity drugs? What do you think are the biggest challenges for patients with obesity?
Dr. Kaplan: I think the biggest challenge is that the drugs don’t work well. If you subject medications to treat obesity to typical efficacy criteria, then they are all wanting; if you apply the less stringent efficacy criteria that we use for weight loss medications, then they work reasonably well. For example, with medications for hypertension or elevated cholesterol, the expectation is that they will bring blood pressure or cholesterol into the normal range. We don’t want drugs that lower high blood pressure from 200/100 mmHg to 190/90 mmHg, because this degree of improvement would be obviously inadequate. Our expectation for most metabolic diseases is that medications will resolve the abnormalities. The problem with obesity is that there are no therapies that reliably bring someone into the normal range. So we are stuck with less complete resolution and less beneficial endpoints, such as several pounds of weight loss. On average, most drugs generate between 4% and 8% weight loss beyond what a placebo would give you. This degree of efficacy is statistically significant and can be clinically valuable, but it is ultimately unsatisfying for both patient and provider alike. If someone weighs 200 pounds and achieves 8% weight loss, that means they lose only 16 pounds, and even that amount of weight loss is usually not maintained.
So the end result is really limited efficacy of currently available medications, which is why they are not particularly successful in the marketplace. In terms of side effects, most of these drugs are pretty safe. Certainly, every drug has its risks, but the biggest challenge is that these medications aren’t as effective as we would like them to be.
Kelly: So even though they are generally safe, it is hard to get people motivated to take them because they don’t have a significant impact?
Dr. Kaplan: Exactly. If I had an obesity problem, what would motivate me to take a drug that provides five or eight pounds of weight loss? Why would I take even a small risk for that modest benefit? As an example, many people focus particularly on the gastrointestinal side effects of orlistat (Xenical [Roche] or Alli [GSK]). As a result, companies are working to develop drugs that work through the same mechanism but without the side effects. If the result of these efforts is a drug with the same efficacy as orlistat, I doubt that it would be successful, despite the improved side effect profile. On the other hand, if you had a drug that was truly effective, but had the side effects of orlistat, people would likely tolerate those side effects. For the currently available medications for obesity, I don’t think that the side effects are the most important reason for their limited use.
Kelly: That’s interesting and a very instructive take on drug tolerability for us.
Sanjay: A related follow-up: when you say a drug that “is truly effective,” are you referring to a particular threshold of weight loss?
Dr. Kaplan: There are published studies that have shown what most patients want in terms of weight loss. Ideally, of course, the drug would work 100%, meaning that the patient’s weight would be normal after taking the drug for a period of time. I don’t think that that outcome is anywhere within the range of possibility right now. More practically, I would like to see double-digit (10% or more) weight loss. Few, if any, of the medications now available or on the horizon will achieve this benchmark. Given their limited effectiveness for the total population of patients with obesity, I would prefer to take a different approach. It seems safe to assume, based on clinical and epidemiological evidence, that there are multiple types of obesity, manifest by differences in the severity of obesity, age of onset, body fat distribution, comorbidities, and other symptoms (hunger, satiety, craving, etc). I would estimate that there are several dozen or as many as a hundred different subtypes of obesity, each of which is likely to respond differently to different therapies.
Therefore, rather than trying to reduce the weight of the entire population, which is highly unlikely to succeed because of the heterogeneity of patients with obesity, I would seek a therapy that has a more profound effect (e.g., causes full remission of obesity) in a small percentage of the population. If you have a therapy that can eliminate or fully control obesity in even 1% of patients, then that population can be taken out of the “at risk” pool. Additional therapies would then need to be developed for the other 99% of the population. With another therapy eliminating obesity in another 1%, we reduce the at risk group to 98% of original population, and so on. I think that given the heterogeneity of obesity, this strategy is more likely to be successful than one that requires a single agent or even a combination of agents to work, even modestly, in the entire population of people with obesity. No such agent has been developed previously, and I don’t think it’s a reasonable expectation, even with the tremendous advances in our understanding of the biology of weight regulation.
Kelly: So there would have to be personalized therapies or technologies?
Dr. Kaplan: Well, it wouldn’t have to be personalized in advance because the beauty of a medication, as opposed to surgery, is that you can try it to see if it works. Even if only 1% of people respond dramatically to a particular drug, if that drug is safe, you could try it in nearly everyone with obesity. The 1% who respond are effectively taken out of the game because their obesity is resolved. For the other 99%, the drug is stopped and you move on to try the next medication. If you have only one medication available, of course, this is not an effective strategy, but if you have 20 to choose from, you can experiment until you find the most effective medication or combination of drugs for each individual patient.
With more therapies available, we have more opportunities for success. We can try one or more drugs in sequence; depending upon the outcomes of these individual patient trials, we can then evaluate whether one or more combinations of drugs or other therapies might be more effective. So we’ll then try various combinations in sequence. This is a highly empirical approach, and there is no magical way of doing it, but I believe it unlikely that a single drug is going to provide a large benefit to more than a small percentage of the population. The likelihood is that two or three-drug combinations will be much, much more effective. This approach makes sense and it’s very attractive, especially when we look at the mechanisms of the one approach that does work – surgery – and recognize that this intervention really embodies a combination of therapies within a single operation. I believe that the most important message from surgery is that to combat obesity successfully, we need to affect this very complex regulatory system at multiple points. At its core, bariatric surgery is a blunt tool that affects multiple nodes of this regulatory network. By contrast, most drugs are more selectively targeted and affect only one node of the network, which is inadequate to reverse the more widespread abnormalities in that network that cause obesity.
One way to think about this complex system is to imagine an orchestra of a thousand players (there are likely to be more than a thousand different genes involved in obesity) in which the players are out of tune with each other. It is unlikely that you will fix the problem by having a vigorous conversation with a couple of second cellos. You might need to retune several dozen or a hundred of the thousand instruments to bring the orchestra back in tune. On the other hand, in rare cases, you might be lucky enough that the only thing wrong with the orchestra is the second cellos and that targeted intervention would be enough. Retuning most orchestras, however, requires the broader intervention, and I think surgery provides that type of broad-based intervention for the physiological dysfunction that leads to obesity; it hits a lot of different parts of the relevant regulatory systems. But there will be that 1% of the population where the major cause of the obesity is directly in line with the effect of the drug, so for that 1%, the drug will be extraordinarily effective. If you take this more individualized approach, looking for the dramatic benefit in a small percentage of the population (what I call the “Pac-man approach” to obesity therapy), then with enough different therapies, you can systematically control obesity in progressively larger subpopulations. Each time you “Pac-man” away even a small subset of patients by providing truly effective therapy, you have made the kind of durable progress that allows focus on the next subset of patients.
drugs and devices in development for obesity
Sanjay: Focusing on the drugs in development for obesity, what innovations are you most interested in? How important is to understand how these new drugs in development work?
Dr. Kaplan: Given our limited understanding, I am not certain that the mechanisms matter as much as whether or not the medication works. While my research is heavily focused on how the drugs work, in the first instant what is most important is that the medication works (in at least a subpopulation of patients) and that it is safe for use in that population. If I had a choice of an effective and safe medication whose mechanism I didn’t fully understand versus a less effective drug whose mechanism I fully understood, I (and most of my patients) would likely prefer the first one. Remember, of course, that most of the emerging medications don’t work any better than the ones we already have. Their greatest opportunity will likely come either from their ability to effectively treat a new subpopulation of patients with obesity or from their ability to work as part of new, combination therapies. Among the emerging therapies, the one that does seem to work better than currently approved medications is Qnexa, which is a combination of two approved drugs, phentermine and topiramate. This combination is commonly used in specialized obesity centers already, since both components are available as single agent.
Kelly: What do you think about the safety of these new drugs awaiting approval from the FDA?
Dr. Kaplan: There is a large school of thought that views obesity as a lifestyle choice, which is not a perspective that I share. Many people who have this perspective, however, believe that any kind of medical therapy for obesity is inappropriate, whether it be surgical or pharmacological, because we typically don’t treat lifestyle choices with medical therapy; we save such approaches for “disease.” People don’t always make this distinction consciously, but to the degree that it is considered inappropriate to use drugs, then virtually no drug would be viewed as safe enough. However, if you consider obesity as a real disease with real medical consequences, some measure of risk would be acceptable. In evaluating treatments for cancer, we commonly accept substantial risks of adverse effects. The question is where we place obesity among the spectrum of diseases. The answer to that question will determine what kind of risks you’re willing to take in treating the obesity. We also must consider the wide heterogeneity of obesity. While some forms of obesity may be potentially deadly, there’s a broad distribution of manifestations. Nearly everyone wants to lose some weight at some point in their life. So there is always a risk that people who have no medical indication will take a particular weight loss drug. This consideration needs to be taken into account when looking at the risks (and benefits) of any particular medication. But the notion that drugs for obesity should be risk-free stems from the perspective that obesity is not worth treating medically at all. If a disease is risky enough to require treatment, it is risky enough to accept some measure of risk from the therapy. The critical factor is the relative risk vs. benefit of the therapy in individual patients.
Dr. Kaplan: This device appears to reproduce one or two of the mechanisms of bypass surgery. I like to conceive of bypass surgery as five operations in one: the isolation of the small part of the stomach, exclusion of the remainder of the stomach, exclusion of the upper small intestine, exposure of the mid and lower small intestine to undigested nutrients, and a partial vagotomy (partial cutting of the vagus nerve to reduce acid secretion in the stomach). Of these five components, only two are reproduced by this device. This device appears to have a profound beneficial effect on diabetes, both in animal models and in early human data. It has a more modest effect on obesity. We can infer from these observations that the intestinal part of the gastric bypass has a greater impact on diabetes. And through other studies, including studies of gastric banding, we can say that the stomach part of the bypass seems to have a greater effect on diminishing food intake. From a clinical perspective, the fact that the EndoBarrier seems to have many of the same effects on diabetes as a gastric bypass is very powerful because this device is a lot less invasive than a bypass.
The device, however, also has its limitations. In its current form, it is not a permanent solution, unlike a bypass, which is permanent. But to have a substantially less invasive approach that accomplishes the same physiology as the bypass, at least with respect to diabetes, makes this a very attractive approach. One of the goals of our research on how surgery works is ultimately to “bypass the bypass.” We hope to discover a less invasive method of achieving the same benefits as a bypass. One way to do this might be with combinations of medications; another way could be to use devices that reproduce all or part of the effects of surgery. The EndoBarrier seems to be a very attractive device for that purpose.
Kelly: Do you think people who aren’t obese, but slightly overweight, will try to use this device?
Dr. Kaplan: There are several studies going on around the world aiming to determine whether people with type 2 diabetes without obesity or with only mild obesity would benefit from gastric bypass surgery. While surgery appears to provide clear benefit for the management of diabetes, the risk of the surgery in this lower weight population is less clear. We don’t know how the risk-benefit relationship will play out in this population. I would argue that there are probably going to be some subgroups of patients, who are relatively thin, who have diabetes, are not well controlled with drugs, and for whom surgery is the right answer, even though they don’t have obesity. If this is true, then it will be very attractive to have a less invasive approach with the same effects on diabetes as bypass surgery.
hot topics in obesity research
Sanjay: Broadly speaking, can you tell us what are you most excited about in the field of obesity research? What have you been most impressed by and what are you looking forward to?
Dr. Kaplan: I have a somewhat biased perspective because I’m very interested in the treatment of obesity and less focused in my own work on prevention strategies. Nonetheless, I think that prevention is critical. There are two major areas that are most particularly exciting in obesity research and are likely to be going to end up being amongst the most productive areas. One is learning how to “substratify” obesity. If obesity is a hundred different diseases, each of which results in having too much body fat, how do we distinguish among those hundred diseases? If we consider cancer – and let’s say there are 200 different types of cancer – nobody debates that each of these different types behaves differently and responds best to different treatment strategies. The differential response of each type of cancer to different treatments reflects the varied causes and mechanisms of the cancer itself. Analogously, understanding the subtypes of obesity in a way that allows us to develop targeted therapies and preventive strategies is critical. As an example, let’s consider that there is a subset of obesity that is primarily caused or triggered by sleep deprivation, more than by overeating or lack of exercise. That subgroup might do particularly well with sleep therapy. If we could identify that subgroup in advance, we could direct sleep therapy to those patients specifically. For other patients with obesity and disrupted sleep, sleep therapy might not be effective, because they have a different subtype of obesity that is not particularly affected by sleep deprivation. This second group of patients might be more sensitive to exercise, another group might be more sensitive to a drug, and yet another group may be sensitive to changes in the type of foods that they consume. Understanding the subtypes of obesity and identifying ways of characterizing these subtypes is critical.
The second major research area that I’m most excited about and that we work on actively aims at understanding how surgery works. The purpose of these studies is not to promote greater use of weight loss surgery. Rather, because surgery, particularly gastric bypass, is by far the most effective and long-lasting therapy for obesity, we need to understand how it works so that we can mimic it less invasively. Copying the effects of surgery without actually doing the surgery is perhaps the most attractive strategy on the horizon. We used to think that surgery worked by physically preventing the patient from eating or causing the patient not to absorb the ingested nutrients. If that were the case, the best we could do would be to copy those mechanical effects. It turns out, however, based on work that we and others have done, that surgery works by changing physiology. It changes physiology throughout the body but particularly it changes the physiology of metabolism and of glucose balance. It changes the physiological control of hunger and satiety, and as a result, it causes weight loss by mechanisms that theoretically could be reproduced without the surgery. While the direct effects of surgery are to mechanically manipulate the bowel, the end result is that a physiological change occurs. If we figure out what mechanisms are involved, we could create the same physiological changes using drugs, foods, devices, or other kinds of approaches to mimic the outcome without having to perform the surgery. I call this “bypassing the bypass” and I believe we will be able to do this in the foreseeable future. In fact, we’ve already made some pretty good progress in this direction. This is an area that few people would have even thought about three years ago, but that is now becoming a very hot area within obesity research. This is why I think we’re going to make a lot of progress over the next several years.
Kelly: We’re very drawn to this idea of “bypassing the bypass” – can you tell us more about that research?
Dr. Kaplan: It has gotten popular in the last three years but we started doing this kind of research in 2002, or even before 2002, shortly after we opened the Weight Center. At the time, my naïve understanding of surgery was that it mechanically blocked food intake, or caused malabsorption. Just using an operation to force people not to eat doesn’t seem like a very good idea so I wasn’t at all optimistic about it. But after we used surgical therapy on a few patients, we rapidly recognized its profound effects. After surgery, patients would return for follow-up care and say things like, “This is amazing. Are you sure the surgeons didn’t operate on my brain because I don’t care as much about food anymore?” “Food doesn’t call out to me the way it did” or “I don’t crave food the way I did.” A few patients spontaneously said, “I crave salads now,” and none of them craved salads before the operation. When you hear comment like that, it suggests that there really may be effects of the surgery on the brain, which of course was not at all what I had expected. I thought that surgery would prevent the patient from eating, in which case it should make them more hungry and cause more cravings, so the effect is the opposite of what I had expected.
Then we did some clinical studies with our patients and found more and more that they reacted as though their physiology had changed. And then, through a variety of approaches, we’ve been able to convince ourselves that this was a truly physiological intervention. We set up animal models of these operations and found that in these animal models, the operations worked just as well as they do in humans. These studies gave us more confidence that is the effects of surgery are not only physiological but that they are not voluntary. None of the animals that we operate on can read magazines or understand ads that suggest they should lose weight. They just respond to the physiological cues within their bodies. Using these animal models, we’ve pretty well proven that the effects of surgery are physiological. Of course, we now need to determine the detailed mechanisms. Surgery probably activates dozens, if not more, mechanisms, we have our work cut out for us.
We entered into this area of research because of what we heard from our patients. When we talked to the patients and really listened, they told us what the experience was like and it became very clear that we were looking at something very profound. It took a while, particularly in the development of these animal models, but now it has gotten to be a popular area and the pace of new discovery is increasing quickly.
bariatric surgery and diabetes
Kelly: From the perspective of people interested in diabetes, it’s been fascinating for us to see how soon diabetes is resolved with many of these surgeries and that goes back to your point about the effects being physiological in nature; could you talk more about this?
Dr. Kaplan: Of course. It wasn’t terribly surprising to us that the effects on diabetes would be physiological because we had already considered and thought that the effects on weight were physiological. But the fact that the diabetes improves within days of the operation, long before there is any significant weight loss, really caused a lot of people to take notice, initially the surgeons and then the rest of us.
The rapid improvement in diabetes is most commonly seen after the bypass-type operations. These operations cause a very rapid initial improvement in diabetes, followed by a slower additional improvement related to the weight loss itself. Gastric banding (reducing the size of the stomach), on the other hand, does not result in the rapid improvement, but generates a slower improvement in diabetes that appears to come from the weight loss itself. These and other lines of research have demonstrated that there are fundamental differences in mechanism among the different operations. I think we now know that the physiological effects of each of the different bariatric operations are quite different from one another.
Kelly: Are there any guides that explain all of the different surgeries and their mechanisms (which are more related to the small intestine or the stomach)?
Dr. Kaplan: The gastric band and the sleeve gastrectomy uniquely manipulate the stomach. The gastric bypass and the biliopancreatic diversion affect both the stomach and the small intestine. There are other operations, mostly used in research studies, that only affect the small bowel. If the only thing manipulated in the operation is the stomach, I call it a “gastric procedure.” If the operation manipulates both the stomach and the intestine, I call it a “combination procedure.” Historically, these procedures have been described as restrictive (for those that affect the stomach) and malabsorptive (for those that affect the intestine), but neither physical restriction nor malabsorption occurs to any significant degree with these operation. We now know that the mechanism of action is primarily physiological.
Kelly: So if a patient comes in now, with diabetes and a BMI of 50, knowing what you know about the physiology of these operations, what would be the incentive for somebody to get an operation that operates only on the stomach as opposed to a “combination” operation that operates on both the stomach and the intestine?
Dr. Kaplan: We rarely recommend anything other than a gastric bypass for patients with diabetes. For patients who have obesity and don’t have diabetes, there are a lot of issues that go into making the decision about which operation to use. For example, the immediate risk of death from a band operation is one-thirtieth as much the risk from a bypass operation. However, it’s a misleading statistic because it turns out that 15-20% of people who are implanted with gastric bands need to have the bands removed. Many of these patients undergo conversion to a gastric bypass. This conversion operation is up to three times as risky as a gastric bypass done as the first procedure. If you look not at the mortality in the first 30 or 90 days after the operation, but at the mortality related to surgery for the rest of the patient’s life, there is much less difference in risk between the two operations.
Kelly: Wow, really?
Dr. Kaplan: Yes, because that significantly increased risk in those 20% of banding patients who have to be converted; when you get the band placed initially, you don’t know whether are you going to be in that 15-20% of people who will have to be converted, so you have to average that future risk over everyone who receives the band. When you do that, it turns out that the band is not that much safer than a bypass over the long term. Therefore, because of the apparently greater benefit of the gastric bypass for treating diabetes, we rarely recommend gastric banding for these patients.
perceptions of bariatric surgery and obesity
Kelly: Do you have patients now that are calling your center who have diabetes but aren’t necessarily very overweight and are specifically interested in having their diabetes resolved through either surgery or a device?
Dr. Kaplan: There has been more and more publicity about this, so yes. There are a number of patients who are quite interested. The notion of using surgery to treat diabetes isn’t yet very well known but awareness is growing and more and more patients and physicians are looking at it.
Kelly: Yes. And what do your diabetes/ endocrinology colleagues think at the Mass General or elsewhere?
Dr. Kaplan: There’s two ways to look at this question. For type 2 diabetes, the endocrinologists are extremely good at managing the disease medically. When they refer a patient to us at the Weight Center, that patient usually needs surgery because they have failed normally effective medical therapy. So it turns out that the Diabetes Center is the largest source of surgical referrals to the Weight Center. I think that this situation is appropriate in that while the Diabetes Center physicians don’t send us that many patients, they know that surgery provides an appropriate and effective back-up strategy for patients who fail aggressive medical management. They understand fully the benefits and risks of surgery and I am confident in their ability to determine when a patient needs this approach. In my other specialty area, gastroenterology (GI), we often care for patients with ulcerative colitis. Ulcerative colitis is a disease that can be cured by removing the colon. This doesn’t mean, however, that when a patient comes to you with ulcerative colitis, the first thing you do is refer them for surgery. You approach the problem using series of medical therapies, but you always know that if these medical therapies fail, surgery provides a powerful and definitive solution. This is the way that I approach surgery for both obesity and diabetes. We start with medical therapies. However, when those therapies are unable to provide an adequate response, we have surgery as a back-up plan. The endocrinologists at our hospital are very aware and supportive of this approach.
It is critical not to oversell the benefits of surgery. Surgery should not be the therapy of first choice for either obesity or diabetes. However, for people with diabetes in whom medical management is inadequate, surgery may ultimately be the right answer.
Kelly: Do you think, as a country, we’re moving more toward a state where obesity is considered a disease and have you seen changes in terms of how it is perceived?
Dr. Kaplan: There are different schools of thought. The insurance companies would prefer not to call it a disease because that would obligate them to provide broader coverage for obesity-related interventions. Food manufacturers would prefer not to call it a disease because doing so might increase the risk of lawsuits related to food causing obesity. Many physicians and surgeons would prefer to call it a disease to improve the likelihood of reimbursement for the care of patients with obesity. So depending on your bias, you’ll approach the question differently. Trying to approach this issue as objectively as possible, I think that obesity is at least as much of a disease as high cholesterol. High cholesterol rarely has direct effects on health and well-being. Rather, it puts you at higher risk of other diseases that can decrease the quality and duration of life. Obesity clearly increases the risk of other diseases that can have devastating effects. It is at least as much of a disease as high cholesterol and hypertension, so there’s no medical reason not to consider obesity a disease.
From a public policy perspective, I think as obesity becomes more and more of a dangerous epidemic, policy makers will eventually have to recognize that whatever you call it, obesity is hurting and killing people and will have to be treated as a disease.
final comments
Sanjay: Dr. Kaplan, do you have any last words of advice for people searching for ways to treat their obesity along with their diabetes?
Dr. Kaplan: I don’t believe that one size fits all. There are many different types of obesity. A lot of obesity therapy is done by trial and error. People need to be willing to experiment with themselves, not in a risky way but in full recognition that what works for your neighbor is not necessarily going to work for you. It is best to work with a physician, dietitian and/or other healthcare professionals who understand that obesity is complicated and that it’s heterogeneous and who work with each patient to develop a lifestyle and treatment plan that is most suited to their individual needs.
Kelly: Dr. Kaplan, thank you so much for all of your generosity!
Sanjay: Thank you, Dr. Kaplan!







