FDA Panel Votes YES to Using Dexcom’s G5 CGM for Insulin Dosing
By Adam Brown
.jpeg) By Ava Runge and Adam Brown
By Ava Runge and Adam Brown
An 8-2 panel vote finds that benefits of using Dexcom’s G5 CGM for dosing insulin outweigh the risks; patient advocates provide compelling testimonies
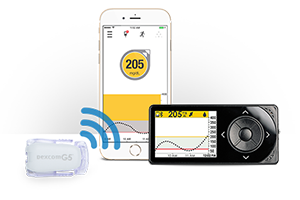
On July 21, an advisory panel strongly recommended that the FDA approve a label update allowing Dexcom’s G5 CGM (continuous glucose monitor) to be used for making diabetes treatment decisions (e.g., insulin dosing) without a confirmation fingerstick. The ten-person panel gave an 8-2 YES vote that the label update is safe; a 9-1 YES vote for effectiveness; and an 8-2 YES vote that the benefits outweigh the risks.
The positive votes make it likely that the FDA will formally approve the label update after negotiations with Dexcom. The two key issues under discussion are: (i) What training will Dexcom need to provide patients and healthcare providers to ensure safe insulin dosing using CGM? (ii) What kind of post-launch study will be required to show that CGM is safe for making diabetes treatment decisions?
The panel discussion appeared confused at points during the meeting, but ultimately, more than 35 compelling patient advocates voiced support for the new labeling. These presentations (highlighted below) provided real life context about using CGM and living with diabetes that gave panel members a comprehensive understanding of the issue, and ultimately, prompted a very positive vote. The panel seemed to view the benefit vs. risk tradeoffs of this label update very positively, and patients and healthcare providers made a particularly strong impact – ensuring that the panel focused away from theoretical points that don’t have too much to do with “real life” diabetes.
The vote is a victory for people with diabetes and the future of CGM, and assuming approval, will:
-
Allow healthcare providers to formally educate users on proper insulin dosing using Dexcom’s G5 CGM (many people dose with CGM already, but don’t receive any education to do it as safely as possible).
-
Bring greater safety for making insulin dose decisions vs. using fingersticks alone (e.g., glucose value every five minutes, trend arrows, alarms).
-
Reduce the hassle of taking confirmatory fingersticks for those already using CGM.
-
Potentially encourage more patients to try CGM and more providers to prescribe it (reducing fingersticks to just two per day makes the technology more compelling).
-
Pave the way for future sensors that reduce or eliminate fingerstick calibrations entirely.
-
Open the door to Medicare coverage of CGM (Dexcom believes Medicare coverage won’t come before 2018, but it can’t happen without this label update).
What did Open Public Hearing speakers share?
During the Open Public Hearing, over 35 patient advocates, including people with diabetes (adults, children, and teens), family members, healthcare providers, diabetes researchers, and professional organizations (JDRF, AACE, ADA, and the Endocrine Society) provided compelling commentary on why this label update will benefit people with diabetes:
-
Dexcom G5 CGM users widely use it for insulin dosing already, meaning this label update simply reflects real-world practice. Additionally, proper education – for people with diabetes and for healthcare providers – can’t occur without an approved label update. Instead of receiving structured guidance and training, people with diabetes are currently learning how to use CGM for insulin dosing via trial and error. Assuming the update is approved, Dexcom will be able to teach when NOT to use CGM for insulin dosing – for example, when a trend arrow doesn’t appear, when there are gaps in data, when symptoms don’t match the CGM readings, etc.
-
Fingersticks are burdensome, subject to inaccuracy from dirty fingers (which can show falsely high blood sugars), and are single, isolated data points lacking the rich context provided by CGM's 288 daily glucose readings, trend arrows, and alarms.
-
Many people with diabetes dose insulin blindly without any glucose data at all – a very big risk with a potentially lethal drug. 80% of people with type 1 diabetes take six or fewer fingersticks per day, and a striking one in three type 1s take three or less fingersticks per day. CGM adds convenience for obtaining glucose data – viewing on a phone or receiver painlessly – which could help address this problem.
-
Only ~30% of type 1s currently meet treatment goals, and lack of fingersticks to guide insulin dosing is a big reason.
-
People with diabetes on Medicare do not currently have access to CGM. Medicare will not consider coverage without this label update.
Quotable Quotes:
-
“My ask is simple. Let’s catch up with the times and have the FDA approve CGM for what it’s already being used for in the real world.” – Manny Hernandez (Livongo)
-
“Approving this label will keep people with diabetes safer and allow proper education for those who are dosing off CGM now from trial and error.” – Adam Brown (The diaTribe Foundation)
-
“CGM gave me proactive information that let me avoid fluctuations and not just react to them.” – Christina Roth (College Diabetes Network)
-
“My wife has not given me glucagon for severe hypoglycemia once since I started on CGM. Before then, it was every few months.” – Lynn Wickwire (Joslin Diabetes Center 50 year medalist)
To watch clips from the Open Public Hearing and panel vote, visit diaTribe’s video archive – The diaTribe Foundation was onsite at FDA and got special permission for this to be the first FDA meeting to use Facebook Livestream. If you're interested in additional content from the Open Public Hearing, you can find Adam Brown's slides here, Kelly Close's slides here and talking points here, Ava Runge's slides here, and 15-year-old Caroline Dorn's talking points here - all have diabetes.
The diaTribe Foundation’s Letter to the FDA
To support this label update, The diaTribe Foundation wrote and sent a letter to the FDA that received nearly 10,000 signatures and over 1,000 comments from patients, family members, advocates, healthcare providers, and researchers. Thank you to all who signed the letter and took the time to share thoughts with the FDA. We were excited to amplify patient voice and help the FDA understand why this label update matters to people with diabetes.
What’s next at the FDA?
On August 29, 2016, the FDA is sponsoring a public workshop in collaboration with The diaTribe Foundation, JDRF, The American Diabetes Association, and The American Association of Clinical Endocrinologists. The goal of the meeting is to identify and discuss diabetes measures beyond A1c to help inform future regulatory processes. Registration for the event is free and open to the public, and attendees will be encouraged to participate both live and via webcast. For more information on the workshop and how you can get involved (including submitting video clips to the FDA!), visit the latest blog post by diaTribe Founder Kelly Close.
(Photo credit: Dexcom)







