How to Keep Your Kidneys Healthy When You Have Diabetes
By Hope Warshaw
 Having diabetes puts you at risk for problems with your kidneys. Learn about the steps you can take, as recommended in the latest ADA Standards of Care, to maintain the health of your kidneys and prevent damage.
Having diabetes puts you at risk for problems with your kidneys. Learn about the steps you can take, as recommended in the latest ADA Standards of Care, to maintain the health of your kidneys and prevent damage.
Your kidneys play an integral role in keeping you healthy. Their main job is to filter waste products out of the body along with extra fluids in the form of urine. The kidneys also play a role to keep blood pressure normal and to make several hormones the body needs to maintain health.
Unfortunately, it’s estimated that 20-40% of people with diabetes develop what’s known as chronic kidney disease (CKD) due, in part, to less than optimal glucose and blood pressure management. Keeping these measures within target ranges, healthy eating and taking medications that help prevent or delay CKD are all actions that go a long way to help keep your kidneys healthy.
Learn in this article how to maintain the health of your kidneys based on guidance from the American Diabetes Association’s Standards of Care for prevention and management of diabetes-related kidney disease.
Click below to jump down to a section:
How does kidney damage due to diabetes happen?
The combination of less than optimal management of glucose and blood pressure over many years can slowly damage the small blood vessels in the kidneys. These damaged blood vessels don’t clear the body’s waste products as well. The inability to filter these waste products in turn cause damage to the kidneys.
The chance of developing CKD increases if you smoke, eat foods high in sodium and salt, are inactive, have excess weight or obesity, have heart disease, and/or a family history of kidney failure. In addition, having CKD can increase a person’s risk for heart and blood vessel diseases.
How to prevent or delay diabetes-related kidney problems
As is true for the prevention or delay of most diabetes-related problems, there are actions to take daily, like keeping your glucose and blood pressure well managed, and actions to take annually or more frequently to detect a problem. Learn more about the actions to take below.
Get and keep glucose in a desired target range
Good glucose management over time can help reduce the risk of or slow the progression of CKD. Work with your diabetes healthcare providers to come up with glucose management targets that are best for you.
If you have type 2 diabetes, talk to your care providers about taking an SGLT-2 inhibitor, such as Farxiga (dapaglifozin), Jardiance (empagliflozin), Invokana (canaglifozin), or Steglatro (ertugliflozin). SGLT-2 inhibitors help prevent the progression of CKD by reducing the amount of glucose that is reabsorbed by the kidneys and increasing the amount of glucose put out in the urine. (Though these medications are being used by some people with type 1 diabetes, they are not approved by the FDA for this use.)
Regarding kidney function specifically, research shows that these medications can reduce weight, blood pressure, albuminuria (see definition below) and estimated glomerular filtration rate (eGFR) (see definition below). Research also shows that SGLT-2 inhibitors can protect against heart failure.
If you have type 2 diabetes and are at an especially high risk for CKD progression or heart disease, talk to your healthcare provider about a relatively new FDA approved medication called Kerendia (finerenone), which can be used alongside SGLT-2 inhibitors. It has been shown to slow the progression of CKD along with having cardiovascular disease benefits.;
Discuss the use of one of these medications with your diabetes care providers based on your individual medical situation, health plan coverage and other factors.
Get and keep your blood pressure at the desired target
Know your current blood pressure and the recommended blood pressure targets. Ask your healthcare providers what blood pressure target is best for you and, if needed, the medication(s) that will best help you hit this target.
-
Get your blood pressure taken at every routine clinical visit. If you have high blood pressure it is recommended that you monitor your blood pressure at home.
-
How to manage your blood pressure: Management of blood pressure depends on your blood pressure results and other heart and blood vessel disease risk factors as detailed below.
-
If your blood pressure is greater than 120/80 mmHg (but lower than 130/80 mmHg), put healthy lifestyle and self-care behaviors into action. Reduce the amount of sodium you consume to less than 2,300 mg/day. Some people, but not all, may need to reduce the amount of potassium they consume.
-
If your blood pressure is at or greater than 130/80 mmHg, put healthy lifestyle and self-care behaviors into action and start to take a blood pressure medication with a goal of achieving a blood pressure target below 130/80 mmHg on a regular basis.
-
Blood pressure medications: There are several classes of blood pressure lowering medications. Two that are recommended as best for people with diabetes to start with are ACE inhibitors and ARBs.
These two classes of blood pressure medications reduce adverse heart and blood vessel problems and prevent or reduce the progression of kidney disease. To slow progression of CKD an ACE inhibitor or an ARB should be used in the maximum amount that you can tolerate without side effects. The use of an ACE inhibitor or ARB is not recommended in people with diabetes who have normal blood pressure and normal kidney function measures, including urinary albumin-to-creatinine ratio and normal estimated glomerular filtration rate. Learn more about these measures below.
To adequately manage blood pressure to achieve your target goal, you may also need to add another class of blood pressure medication, such as a calcium channel blocker or diuretic.
If you take an ACE inhibitor, ARB, and/or Kerendia, your healthcare provider should periodically measure and monitor your creatinine and potassium levels. If you take a diuretic your provider should measure and monitor your potassium level.
Restrict the amount of protein you eat
To prevent and/or slow the onset of CKD and live a healthier lifestyle in general, try, as much as possible, to practice essential healthy lifestyle and self-care behaviors. This includes monitoring protein intake on a regular basis. People with stage 3 (see below) CKD, who do not yet need dialysis, should eat a maximum of 0.32 grams/pound of protein per day but not less than this amount. (For example: this amount for a woman at average height and 140 pounds is around 51 grams of protein/day. For a man at average height and 180 pounds this amount is around 58 grams of protein/day).
Note that this is not a protein restriction. It is the amount of protein recommended for all adults. In comparison with eating higher amounts of protein, this level has been shown to slow progression of CKD. People on dialysis may need more protein to reduce malnutrition.
Get two tests to check kidney function annually
If you have type 2 diabetes or have had type 1 diabetes for five years or more, have two tests done to check your kidney function. Diabetes-related kidney disease can typically develop after having type 1 diabetes for 10 years but may already exist in people with type 2 diabetes when they are diagnosed. If you have been diagnosed with diabetes-related kidney disease, you may need to have these two tests done more often, 1 to 4 times per year.
-
The first test is called a spot urinary albumin-to-creatinine ratio (UACR). It assesses the amount of protein (albumin) that is spilling from your kidneys into your urine.
-
UACR results:
-
Normal to mildly increased: <30 milligrams/gram
-
Moderately increased: <30-299 milligrams/gram
-
Severely increased: > 300 milligrams/gram
-
-
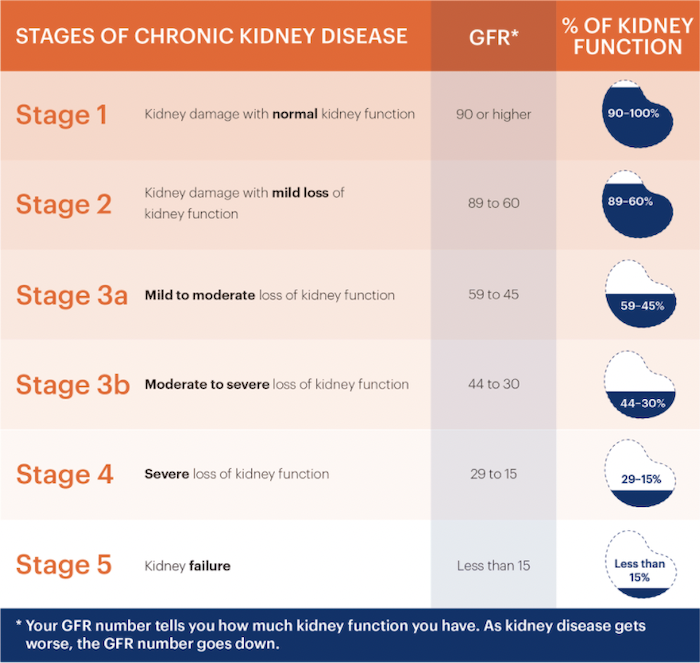
The second test is estimated glomerular filtration rate (eGFR). This measures the rate at which your kidneys are filtering waste products. eGFR is calculated from your age, serum creatinine level, and gender. Creatinine is a blood test that measures the amount of protein that your body is breaking down. An eGFR result of at least 90 indicates normal kidney function. See the chart below for additional details about how eGFR determines the severity of kidney damage.
Stages of chronic kidney disease
Though your goal is ideally to prevent CKD, it is valuable to know about the six stages of CKD.
People with diabetes who are diagnosed with CKD typically, but not always, have had diabetes for many years. Be aware that people diagnosed with CKD generally do not know it until their kidneys are already damaged. This is one reason why it’s so important to get the two regular checks and tests.
People who have continuously increasing urinary albumin levels or continuously decreasing eGFR results should be referred to a nephrologist, a kidney disease specialist. Consulting with a nephrologist at this point has been found to reduce cost, improve quality of care, and delay dialysis.
Treatment options for kidney failure
People who develop stage 5 CKD or kidney failure generally need to start a form of dialysis. There are two types, hemodialysis and peritoneal dialysis. There have been many advances in how and where dialysis can be done. Some people may be able to obtain a kidney transplant for their CKD, but may need dialysis while waiting for a donor kidney. Learn more about kidney transplants.
If you are told you have indications of kidney disease, be sure to take the next steps promptly. Kidney problems will likely progress or worsen over time without treatment.
Perspective from a person with diabetes and CKD
To gain insights into the practical and emotional aspects of diabetes and CKD, we talked to Anne Dalin, 69, who has had type 2 diabetes for about 21 years.
Dalin is a PODS (Part of DiabetesSisters) Meetups co-leader for DiabetesSisters in New Jersey. She is also a tireless volunteer and advocate for the National Kidney Foundation.
Dalin had a heart attack in 2001, at age 48. Initially, damage to her kidneys was apparently caused by the dye used to insert stents in blood vessels around her heart. Soon after her kidney damage was detected, she was diagnosed with type 2 diabetes. Dalin notes that it's likely that she had diabetes for many years before it was diagnosed and that these years of high glucose and blood pressure levels caused kidney disease and progression to stage 4 CKD.
Dalin thought she would need to be on dialysis until she could obtain a kidney transplant. But, as luck would have it, her son was a kidney donor match, and the transplant was done early in 2019.
“Don’t put off the regular checkups and tests to check the health of your kidneys,” said Dalin. “Don’t wait for symptoms, because it’s extremely uncommon to have them until you have significant kidney disease.”
Today, Dalin works hard to keep her diabetes, heart and blood vessels, and her gratefully transplanted kidney, healthy. She carefully watches what she eats and walks regularly. She will always be on medications to suppress her immune system to prevent her transplanted kidney from failing.
“Managing my health is second nature to me now,” she said. “Even if I’m busy, I set an alarm on my phone to remind me to take my medications.”
What works for her may not work for you. What’s most important is that you find what does. Click to view other diaTribe articles about diabetes-related complications.
About this series
Each year the American Diabetes Association updates its Standards of Medical Care in Diabetes based on current science. We’ve translated key points of the up-to-date Standards into plain English so you know how to stay healthy and minimize diabetes complications.
Other articles in this series:








