The Biggest News in Diabetes Technology, Drugs, and Nutrition: Highlights from ADA 2020
By Eliza SkolerJimmy McDermott
 By Eliza Skoler, Jimmy McDermott, Matthew Garza, Divya Gopisetty, Frida Velcani, Emily Fitts, Karena Yan, Joseph Bell, Lorena Bergstrom, and Rosalind Lucier
By Eliza Skoler, Jimmy McDermott, Matthew Garza, Divya Gopisetty, Frida Velcani, Emily Fitts, Karena Yan, Joseph Bell, Lorena Bergstrom, and Rosalind Lucier
The diaTribe team attended the 2020 ADA 80th Scientific Sessions to share several of the greatest highlights from the virtual conference!
The American Diabetes Association (ADA) 80th Scientific Sessions was full of exciting news on advances and studies in diabetes technology, treatments, and nutrition. Click on the links below to learn more!
Diabetes Technology
-
Tandem’s Control-IQ Real-World Data: Time in Range Increases 2.4 Hours Per Day
-
A1C vs. Time in Range – Which Should be Used for Children with Diabetes?
-
Is Technology the Solution to Hypoglycemia? Dr. Bergenstal and Dr. Wilmot Debate
-
Insulin Management Software Glucommander Shows Positive Results on Time in Range
Diabetes Drugs
-
VERTIS-CV Trial of SGLT-2 inhibitor Steglatro on Heart and Kidney Health
-
New Data Shows Teplizumab Delays Diagnosis of Type 1 Diabetes
-
SGLT-2 Inhibitors and GLP-1 Agonists to Prevent Heart Disease
-
Farxiga for Diabetes Prevention? New Analysis of DAPA-HF Trial
-
Metformin, GLP-1 agonists, and SGLT-2 inhibitors in Type 1 Diabetes
-
What Therapies Are Best for People with Type 2 Diabetes at Risk of Heart Disease?
-
The Debate on Metformin and Insulin Use During Pregnancy Continues
Nutrition, Exercise, and Mindset
-
New Physical Activity Recommendations for Adults and Children
-
Diabetes Self-Management Education and Support (DSMES) 2020 Consensus Report Recommendations
-
Real World Stories: Supporting People at Different Stages of Diabetes
Access to Care and Policy
Diabetes Technology
The Next Generation of Automated Insulin Delivery Systems for People with Type 1 Diabetes – Updates from Four New Clinical Trials
The first day of ADA featured data on four clinical trials of the newest automated insulin delivery (AID) systems. In what was a packed (virtual) room, the session began with three highly anticipated presentations of studies on Medtronic’s MiniMed 780G Advanced Hybrid Closed Loop System (AHCL). Dr. Bruce Bode, presented the US adult pivotal trial. Here are the main results:
-
Big news – nearly 80% of participants achieved a time in range of more than 70% without an increase in hypoglycemia.
-
On average, AHCL therapy increased time in range to nearly 75% from a baseline of 68.8%.
-
Among adolescents, time in range increased to over 72% from a baseline of 62.4%.
-
-
AHCL therapy improved average A1C from 7.5% to 7.0%. This is what is sometimes called a “high quality A1C” in the field – hypoglycemia is low, and therefore not contributing to a “better” number.
-
How were these results achieved? Experts said that the lower algorithm target of 100 mg/dl (vs. 120 mg/dl) helped, along with an active insulin time (AIT) setting of 2-3 hours. If you use a pump, check what you have for this setting and talk to your healthcare professional about it to see if you can make changes (regardless of whether your pump can deliver insulin automatically).
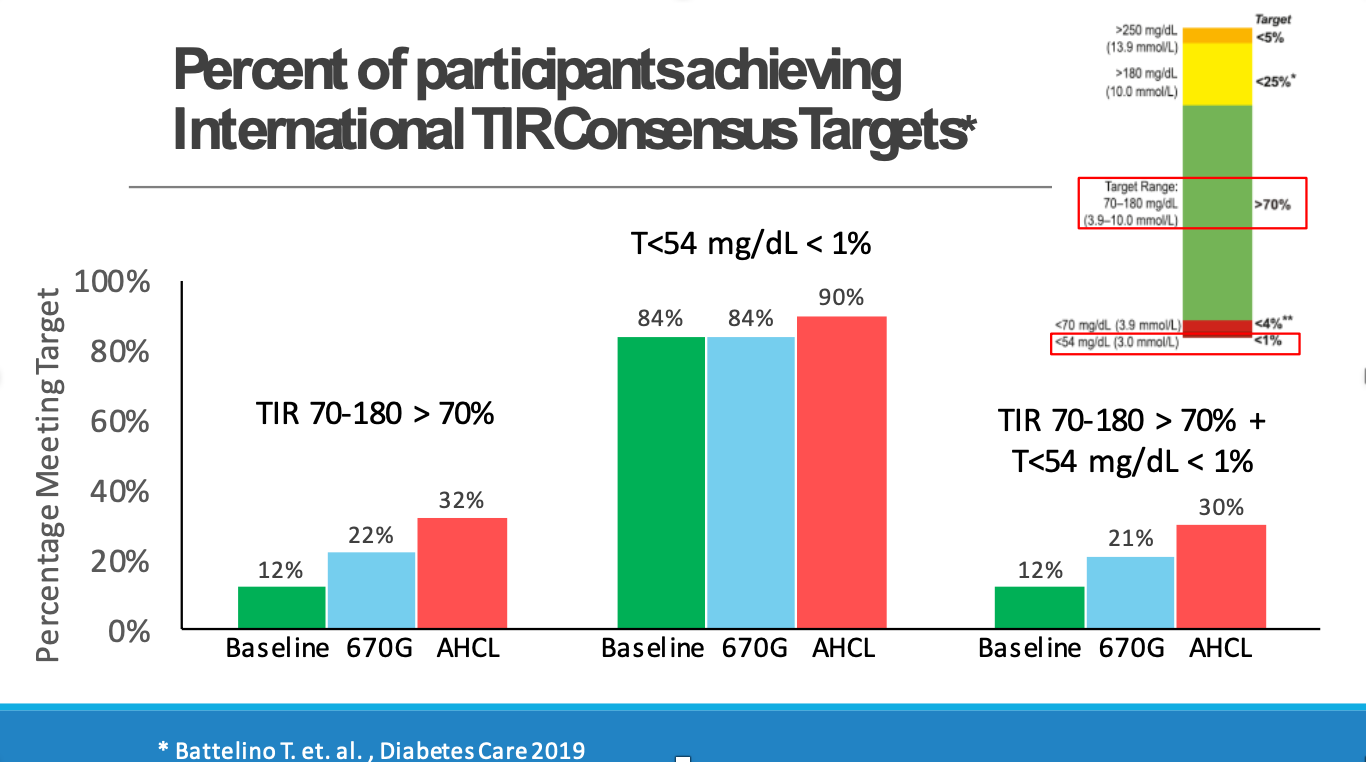
Following Dr. Bode, International Diabetes Center’s Dr. Rich Bergenstal shared data from FLAIR, a trial comparing MiniMed 780G Advanced Hybrid Closed Loop (AHCL) with the 670G Hybrid Closed Loop (HCL) in adolescents and youth with type 1 diabetes (ages 14-29). This is the first ever head-to-head comparison of an AID system with a commercially available AID system. The study also had broad entry criteria: at start, 20% of participants were on multiple daily injections of insulin (MDI), 38% were not using CGM, and 25% had a baseline A1C above 8.5%.
-
Time in range over 24 hours increased from 57% at baseline to 63% with the 670G and to 67% with the 780G. Notably, 6% greater time in range totals nearly an hour and a half more time in range per day.
-
Compared to baseline, the number of participants achieving the international time in range consensus target of more than 70% was nearly two times higher with the 670G and almost three times higher with the 780G (22% and 32% of participants, respectively, compared to a baseline of 12%; see slide below).
-
This was the first time that a study measured participants meeting the combined metric of both time in range greater than 70% and time below 54 mg/dL less than 1% (see slide below). This is important since all therapy – and particulary automated insulin delivery – aims to decrease hyperglycemia and hypoglycemia.
-
From a baseline average of 7.9%, those on the 670G achieved an average A1C of 7.6%, and those on the 780G had A1Cs that fell to 7.4% on average.
-
Both the 670G and 780G were considered safe when evaluating severe hypoglycemia or diabetic ketoacidosis (DKA).
-
Participants satisfaction favored the 780G over the 670G.
Today’s MiniMed 780G data finished with Dr. Martin de Bock’s study, which served as the clinical trial supporting 780G’s CE-Mark submission (and today’s announced approval in Europe). In a study of 59 people (ages 7-80 years, with an average age of 23) who had never used an insulin pump:
-
Average time in range increased to over 70% from 58% (a change of 12.5%) when using the 780G compared to a sensor augmented pump.
-
Overnight time in range increased to 75% from 59% when using the 780G compared to the sensor augmented pump.
-
The improvement in time in range was primarily driven by a 12.1% decrease in time in hyperglycemia (high blood sugar) with the 780G.
It was warming on Twitter to see Dr. de Bock with his three small children while also engaging in Q&A/Chat from their breakfast table. If you’re on social media, follow Dr. De Bock here.
The session concluded with Stanford’s Dr. Bruce Buckingham who presented data on Insulet’s Omnipod 5 Automated Glucose Control System, powered by Horizon. What fantastic data! The study assessed the safety and effectiveness of the fully on-body system over 14 days of use before starting the three-month pivotal study. Interestingly, this study was conducted during the winter holiday season when some of the lowest time in range is observed (typically a three percent drop); the system performed remarkably well in both children and adults, even during this challenging time period.
-
In adults, time in range increased to 73% on the hybrid closed loop system, up from 65.6% using standard therapy – this is the same as nearly two hours more time in range per day.
-
In youth, time in range increased to 70% on the hybrid closed loop system, up from 51% using standard therapy – what an increase, nearly five hours more per day.
These reductions in time in range were mostly driven by a decrease in hyperglycemia. Hypoglycemia was also very low to start. Dr. Buckingham eloquently emphasized, “… this is so important for families and people at night to go to sleep and not worry about hypoglycemia … for a number of kids, they got to go on their first sleepover during this study. It was really decreasing a lot of the burden and a lot of the thinking about diabetes.”
Tandem’s Control-IQ Real-World Data: Time in Range Increases 2.4 Hours Per Day
Tandem presented two posters featuring very positive real-world data from early Control-IQ users. Control-IQ was cleared in December 2019 and officially launched in January 2020.
The first poster, Control-IQ Technology in the Real World: The First 30 days, included at least 30 days of pre- and post-Control-IQ data from 1,659 participants. During the first 30-days of Control-IQ use:
-
Time in range increased by 2.4 hours a day (compared to pre-Control-IQ data) to 78%
-
The time in range improvement was driven by a 9.5% decrease in time spent above 180 mg/dl (that’s 2.3 hours less per day in hyperglycemia – wow!).
-
Average glucose levels fell from 161 mg/dL to 148 mg/dL.
-
Glucose management indicator (or GMI, an estimate of A1C) fell from 7.2% to 6.9%.
-
Users spent 96% of time in closed loop!

The second poster, Glycemic Outcomes for People with Type 1 and Type 2 Diabetes Using Control-IQ Technology: Real-World Data from Early Adopters, looked at 2,896 participants with type 1 diabetes and 144 participants with type 2 diabetes, using at least 14 days of pre- and post-Control-IQ data.
-
Time in range was improved by 2.1 hours per day in the type 1 group to 77%
-
Time in range was improved by 1.4 hours per day in the type 2 group 79%
-
Both groups spent 96% of time in closed loop.
We learned so much at ADA about improving time in range, and we were moved by the power of automated insulin delivery in doing so, since it shows much greater time in range with what sounds like so less work for people and their healthcare teams.
To learn more about Control-IQ, check out the following articles:
A1C vs. Time in Range – Which Should be Used for Children with Diabetes?
A panel discussion of leading experts, moderated by JDRF CEO Dr. Aaron Kowalski, focused on the pros and cons of using A1C and time in range as primary metrics in diabetes care and management for children. As they debated the best marker of glucose management, they attempted to define the ultimate “goal” of diabetes care: is it preventing complications, spending less time in hyperglycemia and hypoglycemia, or improving mental and emotional wellbeing?
Dr. William Winter presented extensive evidence that A1C can predict a person’s risk of developing complications (kidney disease, heart disease, retinopathy, and neuropathy). While lower time in range has been associated with microvascular complications, experts agree that more studies are needed to determine its predictive accuracy for long-term outcomes. Dr. Thomas Danne presented results from the SWEET project that furthered the case for A1C as a measure of population outcomes: setting ambitious targets based on A1C could lead to significant improvements in outcomes for children with type 1 diabetes.
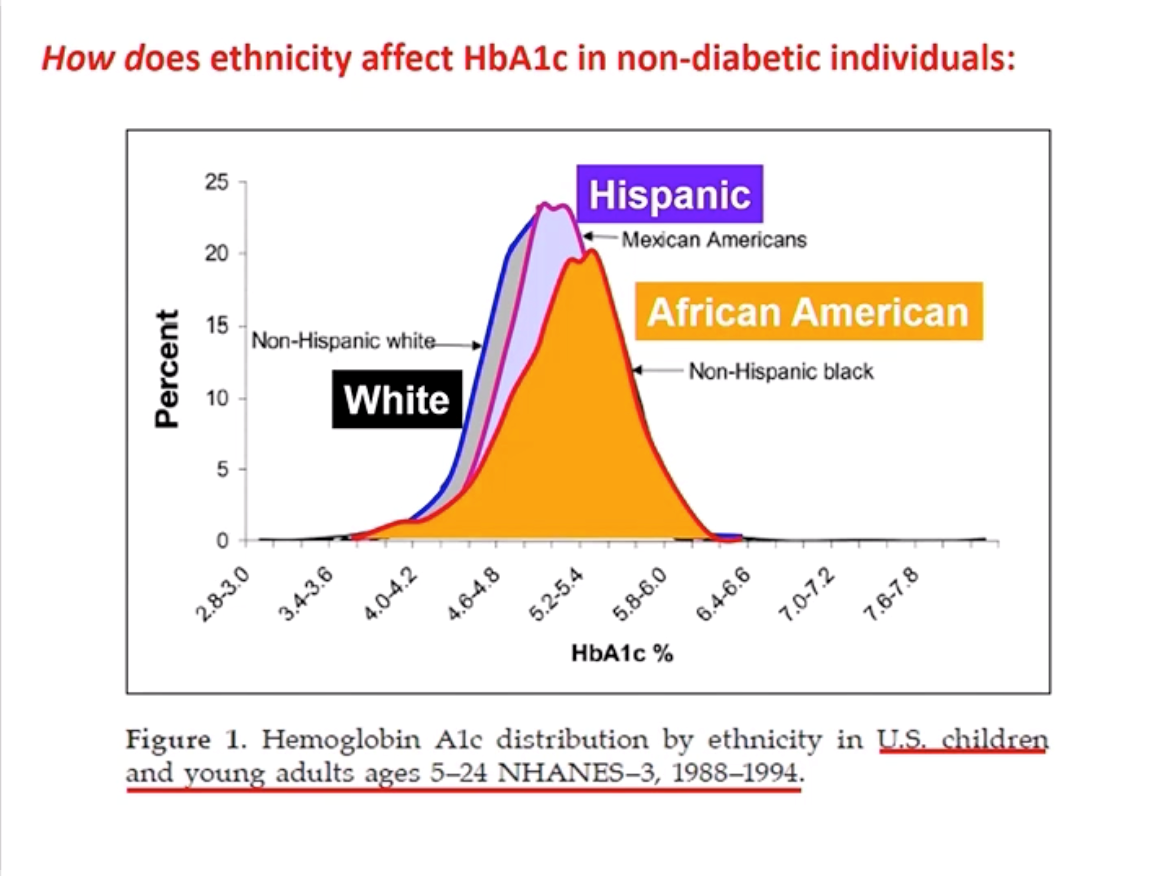
Experts discussed cases in which A1C can be misleading and time in range may emerge as a more reliable measure of glucose control. Dr. Winter explained that population A1cs differ among racial and ethnic groups, leading to misdiagnosis (for example, African Americans have a higher A1c on average compared to white people). Very importantly, as diaTribe has reported on for many years in Beyond A1C research, A1C also does not demonstrate hypoglycemia, hyperglycemia, or glucose variability. According to Dr. Danne, healthcare professionals find CGM reports more helpful in identifying daily highs and lows and in adjusting therapy. This technology allows them to better work alongside families to set individual and measurable goals based on time in range – it is terrific to hear about this continued teamwork.
.jpg)

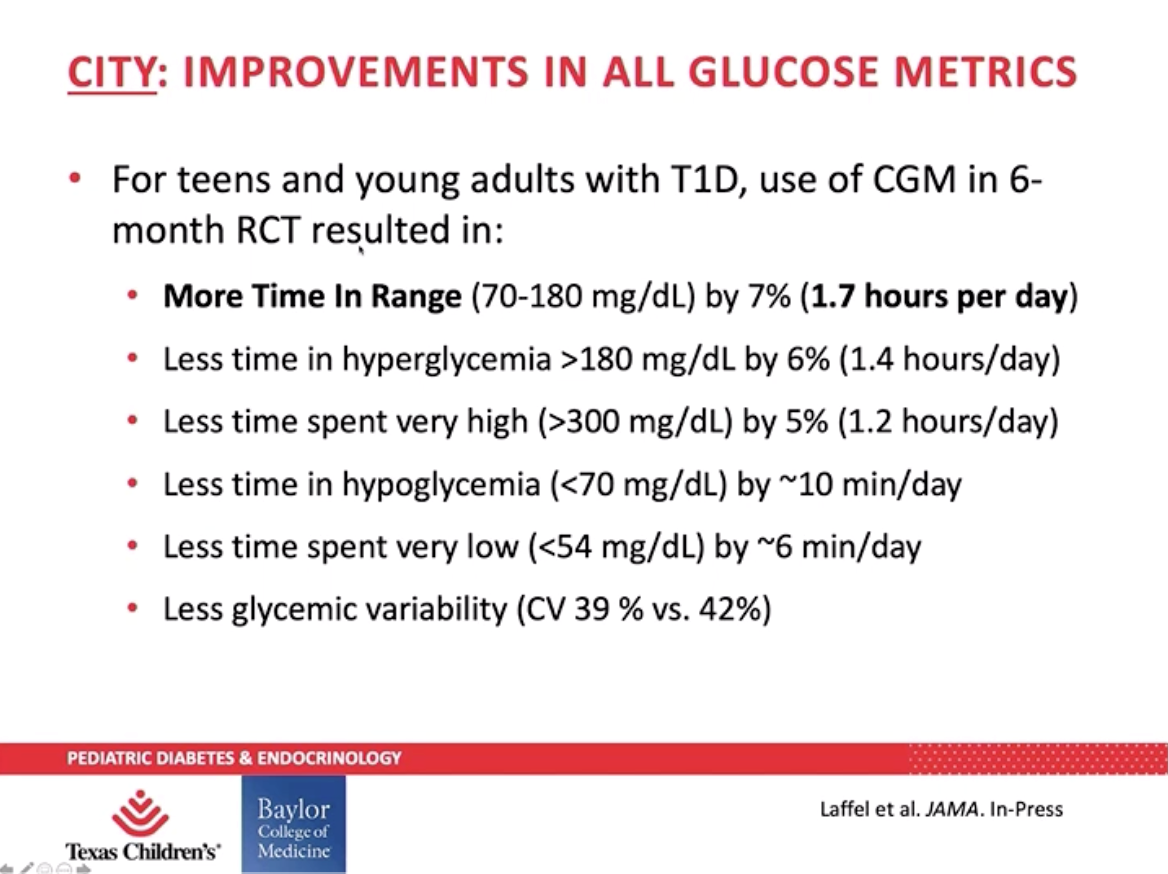
Though Dr. Danne acknowledged the issue of access and affordability, he believes CGM use will continue to increase among children who are tech savvy. Dr. Daniel DeSalvo presented data from the SENCE and CITY to further support use of CGM among children with type 1 diabetes. Young children (two to seven years old) enrolled in the SENCE study saw their hypoglycemia (blood glucose under 70 mg/dL) and time spent over 300 mg/dL reduce by 40 minutes per day – that’s nearly five hours a week. Teens and young adults (ages 14 to 24) in the CITY study saw a 7% increase in time in range, which is almost two more hours per day spent in range – 100 minutes, to be exact!
The Use of CGM in Type 2 Diabetes — Is There Value?
Continuous glucose monitoring (CGM) has been a revolutionary tool; it gives people real-time updates on their blood glucose levels that can help to increase time in range (TIR). For most providers in diabetes, the value of CGM is now nearly universally supported (either “real-time” or “professional CGM”) even if all people with diabetes can’t get it. Reimbursement throughout much of the world has reinforced the value of CGM in type 1 diabetes almost everywhere, though the value of CGM for people with type 2 diabetes is still being explored.
 Dr. Philis-Tsimikas argued for CGM for type 2 diabetes given the technology’s ability to offer remote solutions for care management, provide direct feedback of behavior modification, and allow evidence-based changes to drug therapies. Dr. Philis-Tsimikas shared data from several CGM studies in people with type 2 diabetes on a variety of therapies (basal insulin alone, and oral and other medications), highlighting the improvement in clinical and behavioral outcomes. In what could be the most exciting set of results, people with type 2 diabetes who used real-time CGM (RT-CGM) intermittently for 12 weeks showed an average A1C reduction of 1 percentage point at the end of 12 weeks (compared to a 0.5 percentage point reduction in the blood glucose meter control group). During the 40-week follow up period, A1C was still significantly lower in the RT-CGM group.
Dr. Philis-Tsimikas argued for CGM for type 2 diabetes given the technology’s ability to offer remote solutions for care management, provide direct feedback of behavior modification, and allow evidence-based changes to drug therapies. Dr. Philis-Tsimikas shared data from several CGM studies in people with type 2 diabetes on a variety of therapies (basal insulin alone, and oral and other medications), highlighting the improvement in clinical and behavioral outcomes. In what could be the most exciting set of results, people with type 2 diabetes who used real-time CGM (RT-CGM) intermittently for 12 weeks showed an average A1C reduction of 1 percentage point at the end of 12 weeks (compared to a 0.5 percentage point reduction in the blood glucose meter control group). During the 40-week follow up period, A1C was still significantly lower in the RT-CGM group.
Dr. Elbert Huang gave what we felt was a less persuasive view. He argued that in most cases, CGM use is not valuable for people with type 2 diabetes, on the basis of cost. Howerver this is based on outdated data – just yesterday at ADA, there was striking Late-Breaker data presented that showed very meaningful reductions in A1c by Dr. Eden Miller and Dr. Gene Wright (he’ll be speaking at the TCOYD/diaTribe Forum Monday night!) The study showed very meaningful A1C reductions in thousands of people with diabetes – starting A1C was 8.5%, which fell to 7.6% to 7.9% depending on the population. Dr. Huang presented two studies that showed that the cost ratio of CGM was different depending on the assumptions of costs related to the quality and quantity of lives impacted by type 2 diabetes. A QALY, by the way, is a “quality adjusted life year” that measures both quantity and quality (based on disease burden) of life years. We also strongly believe that many people become more engaged in their diabetes management due to a variety of factors that reduce stigma (no fingerstick tests required, etc.) and enable them to focus on how data and technology can work together to improve their results.
Dr. Huang suggests that less costly treatments (such as the use of ACE inhibitors to avoid high blood pressure or to prevent kidney disease) might be better areas of focus and certainly all experts would agree that focus here is important as well. He also mentioned potential negative psychological effects of constantly checking blood glucose readings using CGM and the fact that this technology may only work if it is shared with a person’s healthcare team – we agree integration with healthcare teams where available is a valuable point and also emphasize our learnings from ADA 2020 from many providers that emphasize, as Dr. Diana Isaacs did on Saturday, that CGM enables greater interest in diabetes management by people. While the technology is extremely important, Dr. Huang also expressed that it could be more valuable if the price of CGM declines or if it is shown to improve glucose management while also reducing the need for costly medicines, among other factors – these factors of cost are extremely important. CGM is going down in price on average and global pricing of $109/month is already available from FreeStyle Libre all over the world. While no one should have to pay $3/day on their own, we believe many more health systems are interested in investing more here due to the positive results they are seeing. We’ll be back with more data from the ADA 2020 Scientific Sessions on this and related fronts!
Parent Perspectives on DIY Closed-Loop
An observational study on Loop, a do-it-yourself (DIY) automated insulin delivery system (AID), used focus groups to gather the attitudes and experiences of parents and children using Loop. The study followed people using an AID system, continuous glucose monitor (CGM) readings, and a communications bridge device, called “RileyLink.”
Overall, parents felt that Loop had a positive impact on their family’s lives. They reported the following outcomes:
-
Improvements in emotional health as a result of a greater sense of security and normalcy, increased quality of life, and decreased parental stress.
-
Improvements in other areas of life, including management of children’s diabetes at school, quality of sleep, confidence in caregivers, and children’s ability to explore extracurriculars without supervision.
Dr. Anastasia Albanese-O’Neill presented survey results on what parents expect of school and diabetes camp staff to help their children manage their DIY closed-loop system. School nurses were also surveyed on their opinions regarding DIY. Here are some highlights:
-
29% of parents expect that school staff will assist children with delivering a bolus.
-
Expectations of diabetes camp staff were lower than school staff – 23% of parents expect school staff to assist with carbohydrate counting and timing of bolus, while only 13% of parents expect diabetes camp staff to do those things.
-
Though 46% of school nurses had never heard of DIY before participating in the survey, 33% of them agreed that school staff should help students using DIY who cannot manage it independently.
This suggests a need for training on DIY and diabetes technology for school and camp staff.
Is Technology the Solution to Hypoglycemia? Dr. Bergenstal and Dr. Wilmot Debate
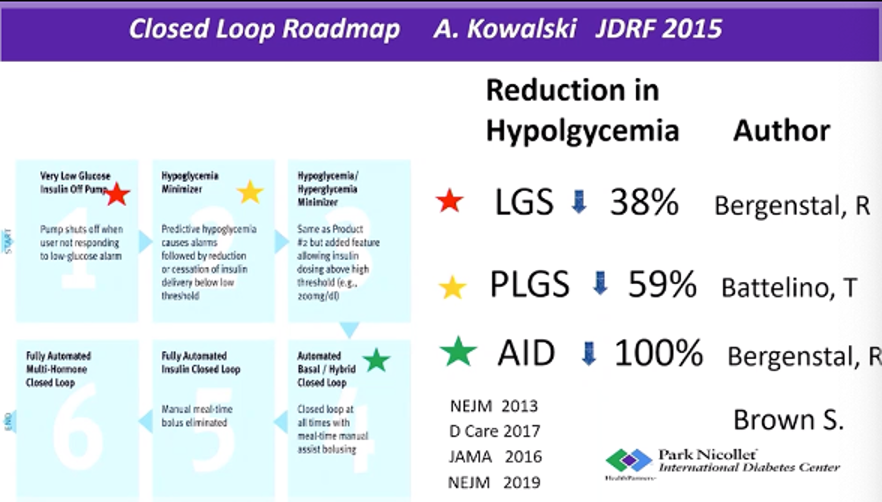
Dr. Richard Bergenstal from the International Diabetes Center (IDC) emphasized the advantages of using continuous glucose monitoring (CGM) for reducing episodes of hypoglycemia (low blood sugar) and other health complications in this debate with Dr. Wilmot. Both doctors are highly regarded, and we took this as a big opportunity to learn lots more rather than land only on one size, though it’s certainly hard to avoid saying yes to this question, from diaTribe’s perspective. Dr. Bergenstal eloquently explained that, on average, hypoglycemia is the biggest barrier to optimal blood glucose management, pointing to the fact that A1C levels increase when people fear going low (what he called the "ripple effect of hypoglycemia"). Luckily, with CGM reports, people can finally detect patterns in hypoglycemia and understand exactly how much time they are spending with blood glucose levels under 70 mg/dL in a day.
Evidence shows that closed-loop technology can reduce and even prevent hypoglycemia. In a study of 124 people with diabetes that Dr. Bergenstal shared, the use of automated-insulin delivery systems (AID) completely eliminated hypoglycemia. This was a historic win – previous studies (see slide below) using low glucose suspend systems (LGS) reduced hypoglycemia by 38%, while predictive low glucose suspend systems (PLGS) reduced hypoglycemia by 59%.
Dr. Emma Wilmot argued that while these findings are exciting, technology is only part of the solution. Technology does reduce the risk of hypoglycemia, but is not available to all (particularly those from underserved populations) and is not suited to all. She said that unless CGM is also paired with structured education, it will not provide the significant and lasting improvements in hypoglycemia awareness that the diabetes community needs. We know, of course, how important education is – and diaTribe will be coming back to discuss this in an upcoming piece about a new article just published in Diabetes Care earlier this week (Diabetes Sisters’ CEO Anna Norton was a key author in the new consensus report)!
Early CGM Use Can Help Kids and Predict T1D Progression
The use of CGM across different populations – including people of various ages and different stages of type 1 diabetes – shows that CGM can accurately predict the progression of type 1 diabetes for people at risk. For those transitioning from “stage 2” to “stage 3”, continuous monitoring can also help prevent DKA, which many people with type 1 have at diagnosis. While there are no clinical guidelines at the moment for how to manage “stage 2” type 1 diabetes, the TESS study is currently evaluating the benefits of CGM use in this population. “Staging” of type 1 diabetes is fairly new and we will be thinking about this more as we consider how to further improve education about type 1 diabetes.

Experts all agreed that earlier use of CGM could result in better diabetes management later on. Dr. Jan Fairchild studied the start and continued use of CGM in a pediatric population with early “stage 3” type 1 diabetes. Kids who started CGM at diagnosis had slightly higher CGM wear at 24 months, compared to kids who started within the first two years of diagnosis (78% vs. 66%, respectively), though this result was not significant. All children using CGM ultimately benefitted – they demonstrated a median A1C of 7.7% at 24 months, which was less than the clinic median A1C of 8.1%. Dr. Fairchild also mentioned the educational role that early CGM use could play, especially with a focus on time in range.
Insulin Management Software Glucommander Shows Positive Results on Time in Range
An exciting study examined the success of the Glucommander insulin dosage software for people with type 2 diabetes on multiple daily injections (MDI) of insulin. Glucommander is an algorithm that helps people with diabetes and their healthcare professionals manage blood glucose levels in both hospital and home settings, using data-driven insulin dosage recommendations. This study focused on the personal use of the software at home.
The study included 25 people with type 2 diabetes who had A1Cs over 8%. The Freestyle Libre 14-day continuous glucose monitor (CGM) was used to measure their blood glucose levels. Participants first received training on multiple daily injection (MDI) basal-bolus insulin dosage, glucose sensors, and nutritional choices. Once they began using Glucommander, the software adjusted recommended insulin doses based on weekly CGM data for four weeks. Participants also received personalized daily meal plans to help them meet their target weight and time in range goals.
The results were positive:
-
The time in range of participants improved week after week throughout the study; overall, the average time in range increased from 48% at the beginning of the study to almost 74% after four weeks.
-
Cases of severe hyperglycemia (blood glucose levels greater than 250 mg/dl) decreased by 19%.
-
Cases of severe hypoglycemia (blood glucose levels lower than 54 mg/dl) decreased by 0.4%. Although this may seem small, it comes out to nearly 40 minutes per week!
-
Total daily insulin use increased by an average of 15.1%, including a 10.5% increase in basal insulin and a 19.7% increase in bolus insulin. This indicates that participants needed to be taking slightly higher doses of insulin to reach their time in range goals.
The results suggest that Glucommander may be a promising option for helping people with type 2 diabetes on MDI basal-bolus insulin improve their blood glucose management outside of clinical settings.
Diabetes Drugs
VERTIS-CV Trial of Steglatro and Heart and Kidney Health
Dr. Samuel Dagogo-Jack and Dr. Christopher Cannon presented highly anticipated results from the VERTIS-CV trial, which studied the effects of Merck/Pfizer’s SGLT-2 inhibitor Steglatro (ertugliflozin) on over 8,000 participants with type 2 diabetes and cardiovascular disease (CVD). The trial found that treatment with Steglatro reduced average A1C by 0.5 percentage points, lowered average weight by nearly five pounds, and reduced blood pressure compared to standard diabetes treatment. Steglatro also improved kidney function, as measured by eGFR, and reduced the number of study participants with heart failure.
The researchers agreed that the VERTIS-CV results confirm the current guidance on the use of SGLT-2 inhibitors to prevent and treat heart failure and diabetes-related kidney disease. As a reminder, the current ADA Standards of Care advise using SGLT-2 inhibitors in people with type 2 diabetes for reducing hyperglycemia (high blood sugar), improving blood pressure, and facilitating weight loss. SGLT-2 inhibitors have also been shown to improve heart and kidney health in people with and without diabetes.
Read more about the trial in our full article here.
New Data Shows Teplizumab Delays Diagnosis of Type 1 Diabetes
At last year’s ADA, we were very excited to report on trial results that showed teplizumab (pronounced Tep-pli-ZU-mab!) delayed type 1 diabetes diagnosis by two years, compared to placebo. The study enrolled 76 participants (55 children and 21 adults) who were the relatives of people with type 1 diabetes and did not have diabetes, and were at high risk for developing the condition (they had unstable blood glucose levels and at least two diabetes-related antibodies). On average, time to diagnosis of type 1 diabetes for the teplizumab group was four years, compared to two years with placebo. At the end of the trial, 53% of the teplizumab-treated group did not have type 1 diabetes, compared to 28% of the placebo group.
New follow up data, presented by Dr. Emily Sims (Indiana University), showed sustained reduction in the onset of type 1 diabetes. Previously, teplizumab had been proven to delay clinical onset by only two years in high-risk people; however, these new data support a delay of as much as three years, compared to placebo.
Furthermore, people who were treated with teplizumab showed a “striking reversal” in C-peptide decline (this is a common measure of type 1 diabetes) in the six months following treatment, after which C-peptide levels seemed to stabilize. These data suggest that the treatment helped stabilize beta cell function (the cells in the pancreas that make insulin) and that repeated teplizumab treatment at key time points may be able to further extend, delay, or even prevent diagnosis of type 1 diabetes. While not a cure, three years of living without daily diabetes management is certainly a meaningful outcome.
When will teplizumab become available? With an estimated six-month review time if Priority Review is granted, an FDA decision could be expected as soon as mid-2021.
SGLT-2 Inhibitors and GLP-1 Agonists to Prevent Heart Disease
Dr. Mikhail Kosiborod (University of Missouri-Kansas City) and Dr. Darren McGuire (University of Texas Southwestern Medical Center) debated the use of SGLT-2 inhibitors and GLP-1 agonists in primary prevention of heart disease (called cardiovascular disease, or CVD).
As background, primary prevention is using medication in people who do not have CVD in order to prevent CVD. This is different from secondary prevention in which a person who is diagnosed with CVD uses a medication to prevent progression of the disease.
Dr. Kosiborod started the session with a strong “yes” – SGLT-2 inhibitors and GLP-1 agonists should be used for primary prevention. However, primary prevention is difficult to prove: larger and longer trials are needed. Dr. Kosiborod believes that we do have enough evidence.
-
A meta-analysis of SGLT-2 inhibitor trials suggests that:
-
SGLT-2 therapy works to prevent heart failure regardless of whether a person has established CVD (based on hospitalizations for heart failure).
-
SGLT-2 therapy protects kidney health regardless of whether a person has established CVD.
-
-
The FDA has approved SGLT-2 inhibitor Farxiga for people with type 2 diabetes and established CVD, and those with risk factors for CVD. That is primary prevention!
-
REWIND showed that GLP-1 agonist Trulicity prevents major adverse cardiovascular events (MACE, which includes stroke, heart attack, and cardiovascular death) in people with and without established CVD.
-
The FDA agrees again here – Trulicity is approved for people with type 2 diabetes with CVD and those with risk factors for CVD.
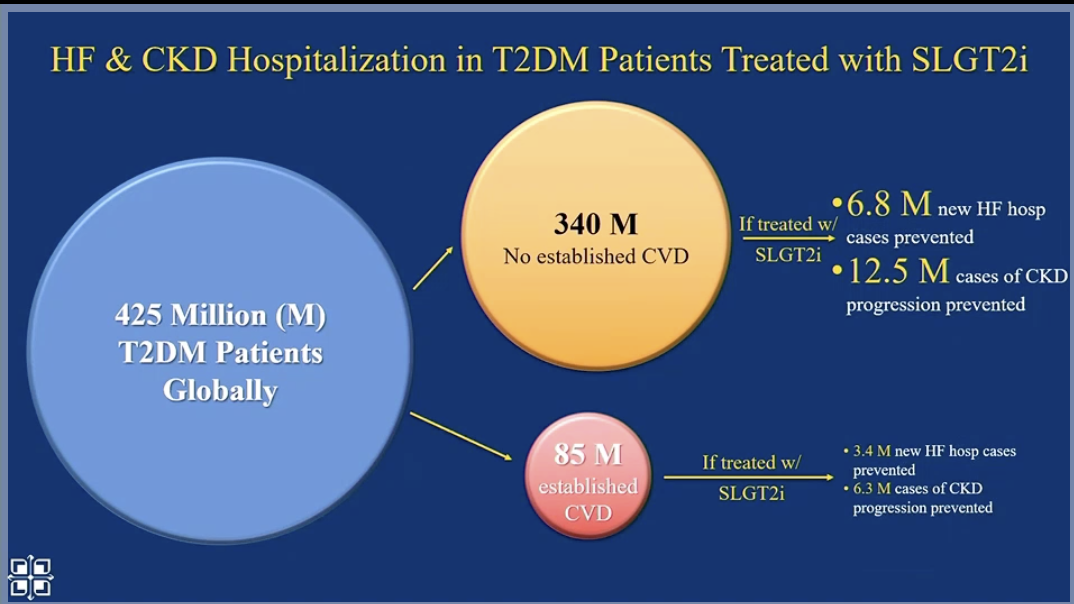
Next, Dr. Kosiborod looked at the population level. Worldwide, primary prevention with SGLT-2s and GLP-1s will significantly reduce cardiovascular events (compared to secondary prevention alone) because there are many people who are not diagnosed with CVD.
Dr. Kosiborod believes this primary prevention is cost-effective and essential, given the high risk to the population. And many SGLT-2s and GLP-1s will become generic in the future.
Dr. McGuire argued that we are not ready for SGLT-2s and GLP-1s to be used in primary prevention. He pointed to a meta-analysis that showed no benefit of SGLT-2 inhibitors and GLP-1 agonists in atherosclerotic cardiovascular disease (ASCVD) outcomes compared to placebo in people without established ASCVD. In his analysis of REWIND, Dr. McGuire pointed to an absolute risk difference of 0.3% in people without established CVD taking Trulicity versus placebo (1.7 events for every 100 patient years, vs. 2.0 events for every 100 patient years). This would mean that you would need to treat 333 people without CVD to prevent one MACE – which would be $3.4 million in drug costs.
Both speakers agreed that SGLT-2 inhibitors have shown strong effects in primary prevention for heart failure and kidney outcomes. There was no significant debate on this point, as the data speak for themselves regarding the profound effect of SGLT-2 treatment in reducing these outcomes.
Weekly Basal Insulin – The Wave of the Future?
New types of insulin – once-weekly basal insulin injections – are being tested in clinical trials and may bring major developments to how people take insulin. In this session, Professor Philip Home, Dr. J. Hans DeVries, and Dr. Stefano Del Prato discussed the pros and cons and recent results from clinical trials of weekly basal insulin.
Prof. Home explained that weekly insulin could reduce hurdles in starting or maintaining insulin therapy for people with diabetes, especially those who are:
-
Afraid of injections
-
Hesitant to start insulin due to the change in lifestyle or impact on quality of life
-
Wary about handling devices
-
Already on a weekly injectable GLP-1 agonist
Weekly insulin could help people adhere to their prescribed therapy – but it will likely make dose titration and adjustments more challenging. One of the major challenges of weekly insulin is that people can’t modify insulin doses according to life disruptions (for example, sick days or increased physical activity).
Dr. DeVries and Dr. Del Prato reviewed the various weekly insulins that companies are studying to evaluate their safety and how they affect diabetes outcomes in comparison to existing insulins. Dr. Del Prato highlighted results from a recent study that compared Novo Nordisk’s weekly insulin (icodec) to Glargine U100 (Lantus) in people with type 2 diabetes:
-
Both insulins showed a similar reduction in A1c.
-
Icodec showed improved glucose profiles for self-monitored blood glucose (SMBG).
-
Rates of hypoglycemia were low for both insulins.
-
Weight gain, which is common when starting insulin, was the same for both insulins.
-
Icodec did not show any new safety issues.
Research is still to come on weekly basal insulin, but it looks promising.
Farxiga for Diabetes Prevention? New Analysis of DAPA-HF Trial
Yale’s Dr. Silvio Inzucchi presented an analysis of the landmark DAPA-HF trial, suggesting that along with the heart health benefits of SGLT-2 inhibitor Farxiga, an additional benefit of preventing type 2 diabetes also exists.
As background, DAPA-HF examined the heart health effects of Farxiga (spelled Forxiga in Europe) in people with and without type 2 diabetes. The trial showed that:
-
Farxiga reduced heart-related death or worsening heart failure by 26% compared to placebo (a “nothing” pill).
-
The heart benefits were the same in people with diabetes and without diabetes.
Dr. Inzucchi’s new analysis showed that for participants who did not have type 2 diabetes at the start of the trial, treatment with Farxiga reduced the risk of developing type 2 diabetes by a whopping 32% compared to placebo. After 18 months, 4.9% of the Farxiga group had been diagnosed with diabetes compared to 7.1% of the placebo group. This is a big deal and anyone you know at high risk of type 2 diabetes should learn about these results and talk to their doctor or healthcare team.
We’re glad to see this important benefit – type 2 diabetes prevention – may be conveyed to people with heart failure who can now take Farxiga regardless of whether or not they have type 2 diabetes. As a reminder, Farxiga is the first SGLT-2 inhibitor drug to be approved for a non-diabetes specific population.
Metformin, GLP-1 agonists, and SGLT-2 inhibitors in Type 1 Diabetes
UCSD’s Dr. Jeremy Pettus moderated a session with three expert presenters from across the world: Dr. Irene Hramiak (Western University), Dr. Tina Vilsboll (Steno Diabetes Center Copenhagen), and Dr. Chantal Mathieu (University Hospital Gasthuisberg Leuven).
 Dr. Hramiak kicked things off discussing the current challenges and risks of insulin therapy, including hypoglycemia, weight gain, glucose variability, and diabetic ketoacidosis (DKA). According to data from the T1D Exchange, average A1C levels have not improved in the last decade, and adolescents continue to be a difficult group for glycemic management, despite increased use of pumps and continuous glucose monitors (CGM). How can adjunctive therapies (added to insulin) help?
Dr. Hramiak kicked things off discussing the current challenges and risks of insulin therapy, including hypoglycemia, weight gain, glucose variability, and diabetic ketoacidosis (DKA). According to data from the T1D Exchange, average A1C levels have not improved in the last decade, and adolescents continue to be a difficult group for glycemic management, despite increased use of pumps and continuous glucose monitors (CGM). How can adjunctive therapies (added to insulin) help?
The REMOVAL study looked at the effects of metformin in people with type 1 diabetes (40 years of age or older). Over three years, participants taking metformin saw the following benefits compared to those taking a placebo:
-
A decrease in A1C of 0.13 percentage points
-
A reduction in insulin dose by 1.2 units
-
No change in the rate of minor or severe hypoglycemia
-
From a baseline body weight of 193 lbs (87.7 kg), a weight loss of 2.6 lbs (1.17 kg)
-
A reduction in LDL (“bad”) cholesterol by 0.13 mmol/L (5 mg/dL)
These data suggest that metformin did not have a clinically meaningful impact on glycemic management but may improve cardiovascular health in adults with type 1 diabetes. That’s disappointing, but something we’ve all wondered for years – now we know!
 Dr. Vilsboll continued the conversation by discussing GLP-1 agonists for type 1 diabetes. She reminded that adjunctive therapy has several important goals but does not replace insulin – which is the main treatment for people with type 1 diabetes.
Dr. Vilsboll continued the conversation by discussing GLP-1 agonists for type 1 diabetes. She reminded that adjunctive therapy has several important goals but does not replace insulin – which is the main treatment for people with type 1 diabetes.
Dr. Vilsboll provided an overview of the effect of GLP-1 drugs in the pancreas (on insulin-producing beta cells), liver, brain, kidneys, and other organs before sharing data from a trial on GLP-1agonists in type 1 diabetes.
The LIRA-1 Study evaluated 24 weeks of GLP-1 agonist use in people with type 1 diabetes and excess weight and found that GLP-1 treatment:
-
Did not have a statistically significant (meaningful) reduction in A1C compared to placebo.
-
Reduced body weight by 13.4 lbs (6.1 kg) compared to placebo (from a baseline of about 205 lbs, or 93 kg).
-
Increased gastrointestinal side effects (nausea, diarrhea).
-
Did not decrease the amount of bolus insulin required but reduced basal insulin by about five to six units per day.
The ADJUNCT trial was the longest such trial, involving 1,400 people with type 1 diabetes with an A1C between 7%-10%. In this trial, participants taking GLP-1 agonists experienced:
-
A clinically significant reduction in A1C of 0.54 percentage points compared to a baseline of 8.2% after 52 weeks.
-
A reduction in body weight that correlated with the dose of GLP-1 agonist: 10.8 lbs (4.9 kg) of weight loss with a 1.8 mg dose of GLP-1 agonist; 7.9 lbs (3.6 kg) with a 1.2 mg dose; and 4.9 lbs (2.2 kg) with a 0.6 mg dose.
-
An increased rate of symptomatic hypoglycemia, but no increase in severe hypoglycemia or DKA.

In a more recent trial, MAG1C, researchers examined the use of GLP-1 agonist exenatide (Byetta) over 26 weeks in adults with type 1 diabetes. Researchers found that compared to placebo, the GLP-1 agonist did not decrease A1C but did decrease insulin dose and body weight. Researchers concluded that the GLP-1 agonist does not have a future as an add-on treatment to insulin in type 1 diabetes. We are not certain this is the correct answer, because it seems like TIR would’ve been useful to measure – but, there’s no fighting city hall.
The session concluded with Dr. Chantal Mathieu discussing the role of SLGT-2 inhibitors in people with type 1 diabetes. She pointed to three main trials: DEPICT with Farxiga, InTANDEM with Zynquista, and EASE with Jardiance.
Compared to placebo, participants taking Farxiga (either 5mg or 10mg dose) experienced:
-
Approximately a 0.45 percentage point drop in A1C by 24 weeks, and 0.2 to 0.3 percentage point decrease in A1C after 52 weeks.
- A time in range increase of about 10% – a gain of almost two more hours of time in range per day

-
A 10% decrease in both basal and bolus insulin.
-
A decrease in body weight of about 5.5 lbs (2.5 kg) with a 5mg dose, and about 7.7 lbs (3.5 kg) with a 10mg dose (from a baseline of 179 lbs, or 81 kg).
-
An increased risk of genital infection and urinary tract infections.
-
No increase in hypoglycemia.
-
An increased risk of DKA that rises with a larger dose.
The inTandem trial also showed a drop in A1C: after 24 weeks, participants taking Zynquista experienced a 0.5 percentage point drop in A1C compared to those taking placebo. Time in range also increased with Zynquista. There was a 77-minute increase in time in range with the 200 mg dose, and almost a three-hour increase for people taking the 400mg dose. The increased risks of DKA and genital infections were also observed in this trial.
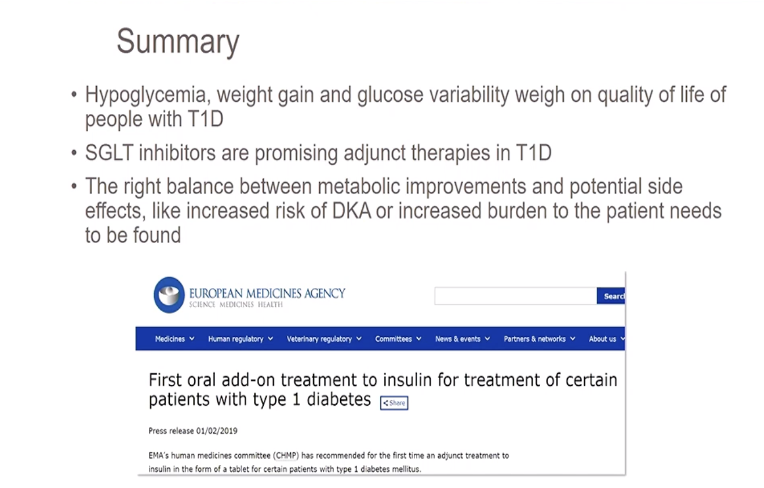 The EASE trial provided evidence that supported the effects of SGLT-2 inhibitors on the reduction of A1C – about 0.3-0.4 percentage points after 52 weeks. This study also used a much lower dose of 2.5 mg, which offered an intermediate effect – lowering A1C by about 0.2 percentage points and reducing body weight by 4 lbs (1.8 kg). Interestingly, there was no difference in DKA with the 2.5 mg dose compared to placebo.
The EASE trial provided evidence that supported the effects of SGLT-2 inhibitors on the reduction of A1C – about 0.3-0.4 percentage points after 52 weeks. This study also used a much lower dose of 2.5 mg, which offered an intermediate effect – lowering A1C by about 0.2 percentage points and reducing body weight by 4 lbs (1.8 kg). Interestingly, there was no difference in DKA with the 2.5 mg dose compared to placebo.
Dr. Mathieu concluded by sharing her “bottom line” on the use of SGLT-2 inhibitors in type 1 diabetes and preventing DKA.
 To learn more about off-label drugs in type 1 diabetes, check out this article from Kerri Sparling.
To learn more about off-label drugs in type 1 diabetes, check out this article from Kerri Sparling.
What Therapies Are Best for People with Type 2 Diabetes at Risk of Heart Disease?
The world of diabetes is now focusing more than ever on preventing diabetes-related health complications. Not only is the treatment of diabetes about blood sugar (measured by A1C or time in range), but it is also about heart health, kidney health, and so much more. In 2019, data from large trials showed that GLP-1 agonists and SGLT-2 inhibitors have heart and kidney protection benefits.
As such, experts strongly emphasized using GLP-1 or SGLT-2 drugs for individuals at high-risk for heart attack, stroke, heart failure, or chronic kidney disease. They also named that GLP-1 and SGLT-2 therapies should become more accessible and affordable to people living with diabetes.
Studies have not yet evaluated the heart and kidney health benefits of metformin, compared to those of GLP-1s and SGLT-2s. However, trials have shown that metformin helps lower blood glucose and body weight, comes with a low risk of hypoglycemia, and is cost-effective.
If your healthcare professional has not brought up additional therapy options for you, we recommend you ask them to read this article and discuss your options.
A Debate on the Use of Sulfonylureas in Type 2 Diabetes
Sulfonylureas, or SUs (drugs like glimepiride, glipizide, gliclazide), are a commonly prescribed low-cost drug for people with type 2 diabetes across the world. At ADA 2020, experts Dr. Sophia Zoungas and Dr. Carol Wysham debated the role of SUs in the treatment of type 2 diabetes. While the two endocrinologists differed on how to interpret data from various studies, we came away from the debate with several important take-aways.
Benefits of SUs:
-
Like many other compounds available today, SUs can help lower A1C, especially at the beginning of use in diabetes management.
-
SUs are low-cost and can be an economical method of managing diabetes, at least in the short term.
-
The CAROLINA study demonstrated that sulfonylurea glimepiride is safe for the heart in people with type 2 diabetes.
Challenges of SUs:
-
The CAROLINA study showed that SUs lead to a greater risk of hypoglycemia than other type 2 diabetes medications (not including insulin).
-
All SUs are associated with weight gain, which itself is associated with cardiovascular disease for many people with diabetes.
-
Not all SUs are created equally – each SU might have different health risks, so more research needs to be done on this front.
-
Preventing long-term complications is possible with GLP-1 agonists and SGLT-2 inhibitors – SUs confers no cardioprotective advantages.
-
Without the cost advantage in the short-term, no one would use SUs.
-
Clinical trial investigators are sometimes discouraged from using SUs in major trials, as we understand it.
If you do use an SU, and have experienced hypoglycemia or weight gain, we encourage you to ask your healthcare professional if there is an alternative. To increase safety, we encourage you to check blood sugar as often as you can (or start using a continuous glucose monitoring device, if you can get access – see here if you are on Medicare) to minimize the risk of hypoglycemia.
The Debate on Metformin and Insulin Use During Pregnancy Continues
Traditionally, healthcare professionals have been advised to use insulin to treat pregnant women who have type 2 diabetes or gestational diabetes (GDM). Now, there is debate about whether metformin or other medications are equally effective alternatives to insulin.
Dr. Denice Feig presented data showing that in pregnant women with GDM, metformin use resulted in less maternal weight gain, less preeclampsia (pregnancy-related high blood pressure), lower birth weight, and less neonatal hypoglycemia (low blood sugar). Additionally, there is no evidence that metformin causes any abnormalities in babies, and the drug may reduce insulin resistance in the fetus. During the first trimester of pregnancy, metformin may be a reasonable alternative, if not a first-line treatment equivalent, to insulin. It is also cheaper, easier to use, and poses less of a risk for hypoglycemia (low blood sugar) than insulin.
While the data are promising, both Dr. Feig and Dr. Linda Barbour pointed out that long-term effects on the baby due to exposure to metformin during pregnancy may include a greater risk of being overweight, developing obesity, and having a higher BMI. Unfortunately, the data did not include pregnant women with type 2 diabetes; an ongoing study, MiTy, is currently studying these effects. Both Dr. Feig and Dr. Barbour emphasized that we need more data to decide the best treatment for pregnant women with diabetes – that may well be, and we also hope that better screening is in the works, so that those at risk of gestational diabetes can learn about it earlier and work with their healthcare teams to live with it successfully, which is eminently possible. Learn more about gestational diabetes in our recent article by Cheryl Alkon.
At the ADA Scientific Sessions this year, Dr. Bruce Bode shared interesting findings from a study measuring the effect of combined insulin-glucagon therapy on blood glucose levels of people with type 1 diabetes. Patients were given either insulin and glucagon or only insulin, and then observed for six hours after eating. The study found that the combined treatment helped prevent hypoglycemia. Compared to insulin-only participants, participants given insulin plus glucagon showed:
-
11% less time below 70 mg/dL.
-
27% fewer hypoglycemic events requiring glucose treatment.
-
An average lowest blood glucose of 114 mg/dL (vs. 51 mg/dL in the other group).
Most importantly, the treatment reduced hypoglycemia without increasing hyperglycemia. There was no significant difference in the post-meal blood sugar “spike” between the insulin-only and insulin-glucagon groups. This suggests that glucagon does not increase the risk of high blood sugar. This is great news on the technology front – it opens the door for new treatments that more closely mimic the human pancreas. We anticipate more “artificial pancreas” devices coming soon; the Beta Bionics iLet (presented at ADA 2019) has already shown promising results using a bi-hormonal system.
In other glucagon-related news, Dr. Kasia Lipska presented data on glucagon usage among U.S. adults with type 1 diabetes (T1D) and type 2 diabetes (T2D). The study found that prescriptions for glucagon were rarely filled by either group (only 1.45% of people with T1D and 0.70% of people with T2D). This is surprising data – most people with diabetes are encouraged to have glucagon available for low blood sugar emergencies.
Further investigation is needed to explain these patterns, especially among people with type 1 diabetes. It’s clear that we need to focus on improving glucagon access for people at high-risk. Dr. Lipska did not discuss the barriers to accessing glucagon, which may explain why the percentage is so low for people with diabetes.
Nutrition, Exercise, and Mindset
New Physical Activity Recommendations for Adults and Children
Dr. Katrina Piercy and Dr. Ronald Sigal presented the 2018 Physical Activity Guidelines for Americans, with updates to the age-specific guidelines and evidence of even more health benefits. These are the recommendations for each age group:
-
Children ages 3-5 should be physically active throughout the day to support their growth, development, and motor skills. Though the US guidelines do not include a specific amount of time, Australia, the United Kingdom, and Canada recommend three hours per day.
-
Children ages 6-17 should do at least 60 minutes a day of moderate or vigorous physical activity.
-
Adults (under age 55) should do at least 150 minutes (2.5 hours) to 300 minutes (5 hours) each week of moderate-intensity activity, or 75 minutes (1 hour and 15 minutes) to 150 minutes (2.5 hours) each week of vigorous-intensity aerobic physical activity. Adults should also do muscle-strengthening activities at least twice a week. We were slightly surprised not to see adults urged to exercise every day like former head of CMS/FDA Dr. David Kessler does in his recent acclaimed book, Fast Carbs, Slow Carbs.
-
Older adults (above age 55) should do the recommended aerobic and muscle-strengthening activities for adults. They should also incorporate balance and functional training, such as standing on one foot or ballroom dancing.

How do you determine the intensity of exercise? Dr. Piercy recommends the “talk test”: someone doing moderate-intensity aerobic activity can talk, but not sing, during the activity, while a person doing vigorous-intensity activity cannot say more than a few words without pausing for breath.
The speakers noted that while the most health benefits come with at least 150-300 minutes of moderate physical activity per week, any activity is beneficial: any time spent sitting that is swapped out for exercise (even light activity,) can lead to short-term and long-term health benefits. Read more about the guidelines here.

Diabetes Self-Management Education and Support (DSMES) 2020 Consensus Report Recommendations
A group of educators made a strong case for the greater use of diabetes self-management education and support (DSMES). The benefits are many, including improvements in clinical, behavioral, and psychosocial outcomes, and greater diabetes knowledge and self-care behaviors. Dr. Margaret Powers stressed that compared to other treatments prescribed by healthcare professionals, DSMES and medical nutrition therapy produce few to no negative side effects for people with diabetes and are low cost.
.png)
The experts discussed low DSMES participation rates across the nation and the factors that reduce referrals to diabetes education. Evidence shows that less than 5% of people newly diagnosed with diabetes who have Medicare insurance, and 6.8% of privately insured people with diabetes, have used DSMES services. The 2020 DSMES Consensus Report was created to address these concerns by outlining steps healthcare professionals can take to help people access DSMES services. The report recommends that healthcare professionals make referrals and encourage participation in DSMES at four critical times in someone’s diabetes journey: (1) diagnosis, (2) annually or when not meeting treatment targets, (3) when complicating factors develop, and (4) when transitions in life and care occur. It also suggests that awareness of, and access to, DSMES must be expanded (culturally and geographically), and financial support should be provided for use of DSMES services..png)

Food as Medicine! Geisinger’s Fresh Food Farmacy
Michelle Passaretti (Geisinger Health System) presented data on the success of the Fresh Food Farmacy initiative. Fresh Food Farmacy was developed to meet the health needs of people with diabetes in Pennsylvania who do not have access to healthy foods (also known as being food insecure). diaTribe interviewed two leaders from Geisinger in 2018, Dr. Andrea Feinberg and Allison Hess; now, Fresh Food Farmacy has provided 482,219 total meals.
The data speaks to the power of food as medicine! The program participants had a:
-
2 percentage point reduction in A1C from a baseline of 9%
-
27% reduction in fasting glucose
-
13% reduction in cholesterol (including a 9.9% reduction in “bad” LDL cholesterol)
-
15% reduction in triglycerides
Fresh Food Farmacy also led to increased use of preventive care: flu shots increased by 23%, annual eye exams increased by 17%, and annual foot exams increased by 33%.
Compared to eligible individuals who did not participate, Fresh Food Farmacy participants saw:
-
49% lower hospital admissions rates
-
13% decrease in emergency department visits
-
27% more primary care visits
-
14% more endocrinologist visits
Participant surveys show significant improvements in quality of life, with 31% of people in the program rating their overall health as very good, compared to just 6% before participation. Additionally, 44% of Fresh Food Farmacy participants now rate their emotional and mental health as very good, compared to just 9% before the program. Passaretti emphasized that Fresh Food Farmacy is not a diet, but a lifestyle change, and that support for the individual’s entire household is necessary for success.
A Sneak Peek into the Film Blood Sugar Rising
Blood Sugar Rising is a film that powerfully articulates the need for a war on diabetes. During this panel moderated by our own Kelly Close, we heard from ADA CEO Tracey Brown, Rise and Root urban farmer Karen Washington, social media influencer and film star Nicole Egerer, film director David Alvarado, and incoming ADA Chief Scientific & Medical Officer Dr. Robert Gabbay.
 Many myths exist in diabetes. One is that if you get diabetes, it is your fault. Blood Sugar Rising dismantles some of these false narratives by showing the complexity of the disease and amplifying diverse voices of people in the diabetes community. Watch the film here if you are in the US and here if you are outside the US.
Many myths exist in diabetes. One is that if you get diabetes, it is your fault. Blood Sugar Rising dismantles some of these false narratives by showing the complexity of the disease and amplifying diverse voices of people in the diabetes community. Watch the film here if you are in the US and here if you are outside the US.
Tracey Brown ended with a powerful call to action: “What will we do when the burning bush stops burning? We need to move from words into action. We get one point for saying and nine points for doing. Each of us can use our voice, our monetary power, and our ears, and reach across the aisle to collaborate. This is what we need to do to bring diabetes down. We can make it happen, but only together. I’m full up of hope and courage that tomorrow is going to be better than today.”
Lifestyle Interventions for Type 2 Diabetes Remission
In a fascinating session on type 2 diabetes remission, several leaders in the field introduced data on how specific lifestyle interventions (diet and exercise) may help put type 2 diabetes into remission.
Alison Barnes presented data from the DiRECT trial, which focused on low-calorie diets (LCD). The trial compared an intervention group on an LCD (between 800-900 calories per day) to a control group receiving typical diabetes care. Remission was defined as achieving an A1C below 6.5% and stopping all diabetes medications. Results from the DiRECT trial were promising:
-
At one year: 4% remission in control group and 46% remission in the intervention group.
-
At two years: 3% remission in control group and 36% remission in the intervention group.
-
64% of participants who lost more than 22 lbs (10 kg) were in remission at two years.
-
The intervention group dropped from 75% of participants on diabetes medications at baseline to 40% at two years (compared to 77% at baseline and up to 84% in the control group).
-
Average A1C decreased by 0.6 percentage points in the intervention group at 2 years.
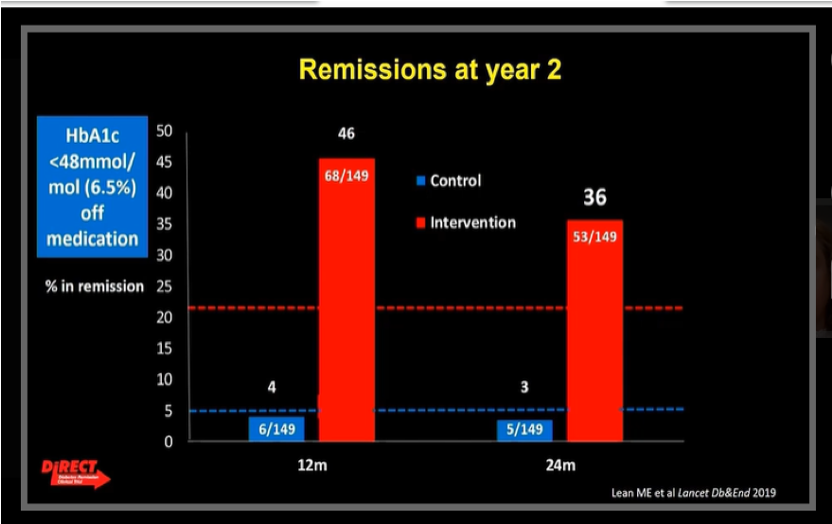 We thoroughly recommend Dr. Roy Taylor’s book Life Without Diabetes: The Definitive Guide to Understanding and Reversing Type 2 Diabetes – he provides a major connection to the DiRECT trial.
We thoroughly recommend Dr. Roy Taylor’s book Life Without Diabetes: The Definitive Guide to Understanding and Reversing Type 2 Diabetes – he provides a major connection to the DiRECT trial.
Next Dr. William Yancy spoke on low-carbohydrate diets (classified as less than 130 g carbs per day, with no overall calorie restrictions). In an analysis that compared the effects of nine different diets on glycemic outcomes in type 2 diabetes, the low-carb diet was ranked as the most effective dietary approach for lowering A1C.
Finally, Dr. Kristian Karstoft presented the U-TURN study on how exercise alone, or exercise and diet, may play a role in type 2 diabetes remission. U-TURN had two groups, one receiving standard care and one receiving intensive lifestyle intervention, which included diet and exercise components.
-
After 12 months, 37% of participants in the intervention group stopped using glucose-lowering medication and maintained glucose levels below the criteria for type 2 diabetes (effectively achieving remission).
-
Of the participants who achieved remission, the majority of them came from the group that consistently exercised the most.
The Need for a Personalized Approach to Obesity Treatment
Experts shared the latest data on different treatments for obesity. They focused on three approaches:
1. Lifestyle interventions:
-
The Look AHEAD trial tested whether reducing calories and exercising regularly would lead to diabetes remission. After one year, 11.5% of participants achieved diabetes remission with an average weight loss of 19 pounds (8.6 kilos). After four years, 7.3% of participants were able to maintain remission with an average weight loss of 10 pounds (4.5 kilograms).
-
The Diabetes Remission Clinical Trial (DiRECT) tested whether calorie restriction alone had an effect on diabetes remission. After one year, 46% of people in this study with type 2 diabetes achieved remission; after two years, 70% of the people who had achieved remission were able to maintain remission.
Participants in Look AHEAD had more advanced diabetes than in DiRECT, leading to the big difference in remission rates. The speakers emphasized that the longer someone has been diagnosed with diabetes, the harder it is to achieve diabetes remission.
2. Obesity medication:
-
Just 2% of people living with obesity are managing the disease with medication. However, many obesity medications can lead to weight loss, prevention of diabetes, and diabetes remission.
-
Combination therapy has shown success for managing obesity and type 2 diabetes. A study testing tirzepatide (a dual GLP-1 and GIP receptor agonist) in people with type 2 diabetes found a 1.7-2% decrease in A1C and an average weight loss of 12 pounds in just 12 weeks.
3. Bariatric surgery:
-
Experts agreed that bariatric surgery should be considered as a treatment option for people with a BMI greater than 35. Bariatric surgery can also lead to sustained weight loss and a decrease in diseases associated with obesity, including sleep apnea and heart disease.
-
It’s clear that obesity treatments must be determined at individual levels – we know that so much more is possible for people with diabetes to reach healthier weights and will be returning to this topic. In the meantime, if changing your weight is of interest, talk to your doctor about how to do this in the best way for you.
How Might Type 1 Diabetes Affect the Gut Microbiome? How Can We Use the Gut Microbiome to Treat Type 1 Diabetes?
Though the science is not yet conclusive, research continues on the relationship between the gut microbiome (made up of all the bacteria that live in the human digestive tract) and type 1 diabetes autoimmunity. Dr. Eric Triplett reviewed studies of the gut microbiome in babies with high genetic risk for type 1 diabetes. Three of the studies (DIPP, Babydiet, and DIABIMMUNE) showed an association between the species of bacteria living in the gut and the onset of type 1 diabetes. He then presented a study using data from the general population in Sweden (ABIS), which compared the gut microbiome of children with low, neutral, or high genetic risk for type 1 diabetes. The study found that high genetic risk for type 1 diabetes is associated with changes in the gut microbiome early in life.
Dr. Emma Hamilton-Williams shared unpublished research on the effect of high-fiber dietary supplements on gut microbiome composition and diabetes management in 18 adults with type 1 diabetes. Fibrous food breaks down into short-chain fatty acids (SCFAs) when digested. SCFAs are known to support gut health and regulate the immune system. The study found that the high-fiber supplements affected the species of bacteria living in the gut as well as their function (though these returned to baseline after the diet ended). Participants with better-managed diabetes at baseline had a stronger response to the dietary change – and experienced changes in their glycemic management: A1C levels decreased and less daily insulin was required. Further research on short-chain fatty acid supplements could shed lead on diabetes treatment and prevention.
Real World Stories: Supporting People at Different Stages of Diabetes
Dr. Neesha Ramchandani presented her work on young adults living with diabetes (ages 18 to 30). Through interviews, she found four main challenges: finding a balance between diabetes and life, feeling in control of diabetes, navigating the hidden burden of diabetes within their social circles, and wanting a better connection with their diabetes healthcare professional. One participant said, “Diabetes is like having a full-time job… you can’t 100% turn off. It always has to be a part of your thought process.” diaTribe has resources for teens here.
We then heard from Dr. Della Connor and Dr. Gary Rothenberg on the need to care for people who are living with diabetes post-kidney transplants and post-amputations. In all three talks, the experts emphasized the need to:
-
Build trust and comfort between people with diabetes and healthcare professionals.
-
Incorporate perspectives based on gender, race, and ethnicity into care.
-
Recognize the importance of a team approach, including care-partners.
Access to Care and Policy
Dr. Lisa Powell (University of Illinois at Chicago) presented compelling evidence in support of sugar-sweetened beverage (SSB) taxes and their ability to reduce soda consumption. Evidence suggests that taxes do reduce the consumption of sugary beverages – a 38 percent reduction in Philadelphia, PA and 21 percent reduction in Seattle, WA, for example – and incentivize soda companies to decrease the amount of sugar in their products, especially when the tax is dependent on the drink’s sugar content. Research also shows that while some consumers replace sodas and sugary drinks with other forms of sugar, such as candy or chocolate milk, the most common substitute is water.
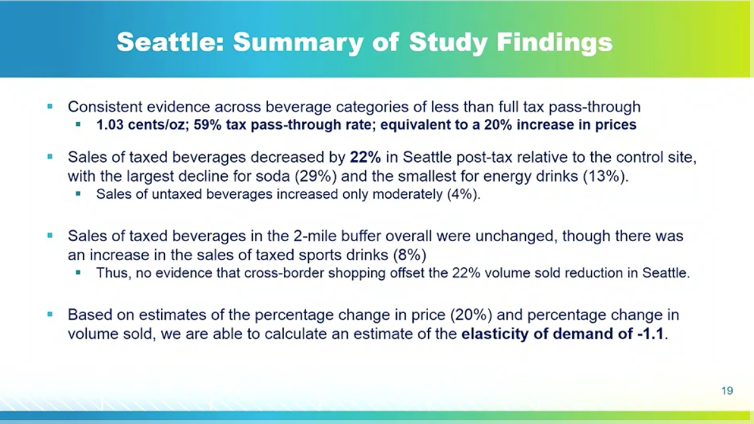
Dr. Martin White (University of Cambridge) and Dr. Rafael Meza (University of Michigan) presented promising data on how SSB taxes are working in the United Kingdom and Mexico, respectively. UK consumers overall have been switching to drinks with less sugar and most companies have been reducing levels of sugar in their products; however, taxes have not had a dramatic negative impact on the sugary beverages industry’s revenues overall. Similarly, Dr. Meza showed that Mexico’s overall sugar consumption has decreased since the implementation of the SSB tax, having the largest influence on people who drink lots of sugary drinks, and he noted that the current tax, which is about 10% of the beverage price, would have a significantly larger impact if doubled.
Dr. Powell pointed out that the most effective taxes require careful design. To significantly curb consumption of sodas, the SSB tax should be added into the shelf price, rather than applied at the register, and the tax ought to apply to a broad base of sugary-drinks (including sodas, juices, sports drinks, etc.) to avoid substitutions. Moreover, researchers must be mindful of cross-border shopping – this is when consumers purchase their beverages in places where the SSB tax doesn’t apply. This tax avoidance can heavily impact the effectiveness of the tax: for example, in Philadelphia, PA, consumers buying SSBs outside of Philly reduced the the impact of the tax from a 51% reduction in SSB sales to a 38% reduction.
Effects of Health Policy on Diabetes Care
Professor Rebecca Myerson (from the University of Wisconsin) shared key findings of a study on the impact of Medicaid expansion for people with diabetes:
-
Medicaid prescriptions for insulin increased by about 40%, even with rising insulin prices, meaning that more people with diabetes are receiving treatment.
-
Prescriptions for metformin also increased, suggesting that more people are getting treatment for early-stage diabetes.
-
About one-third of the other prescriptions are for newer medicines (such as SGLT-2 inhibitors and GLP-1 agonists) – promising trends for preventing diabetes complications and saving significant costs down the road.
Dr. Kasia Lipska from Yale School of Medicine discussed the importance of coverage for essential medicines and pre-existing conditions – two health policy issues that are front of mind for many Americans as the November election approaches. In addition to Medicaid expansion, the Affordable Care Act (ACA, or Obamacare) provided coverage for “Essential Health Benefits,” which includes prescription drugs, mental health services, emergency services and hospital care, preventive services and chronic disease management, and more. Dr. Lipska shared a study that found the ACA reduced the percent of income spent on family medical costs for people ages 18-64 with diabetes. This reduction was especially true for people whose family income was in the lowest bracket ($0-34,999 per year).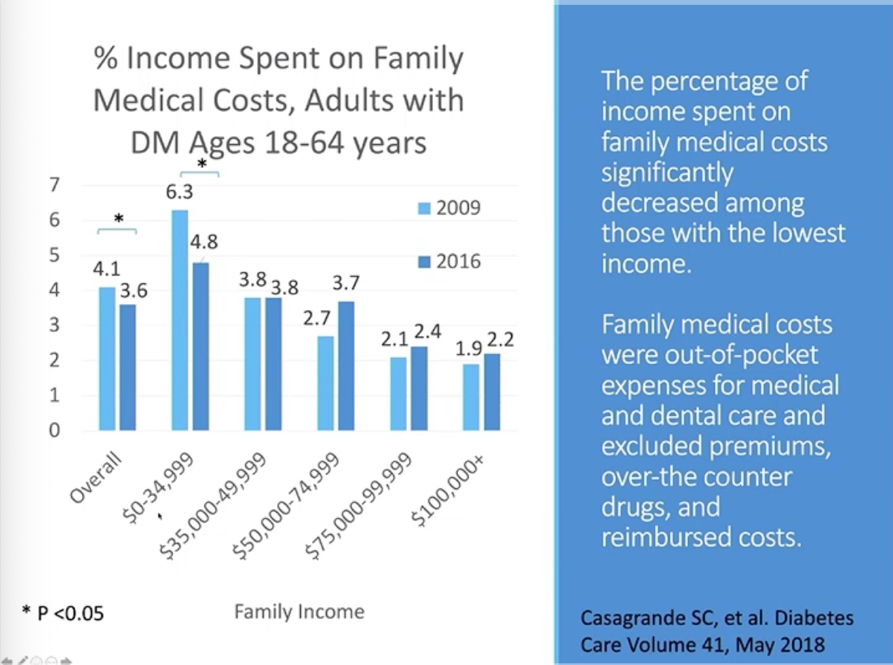
Importantly, ACA also prohibited health insurance companies from denying people coverage or charging higher costs to people who have “pre-existing conditions,” including diabetes. Given the significant improvements in coverage and care, Dr. Lipska emphasized that getting rid of the pre-existing conditions provisions would be “a disaster for people with diabetes” – presumably diaTribe readers in the US would agree! Over half of those surveyed were in favor of expanding Medicaid programs in their state – this doesn’t surprise us, since there are so many states that do not have favorable diabetes care programs (for example, see our article on CGM coverage for people on Medicaid; although this was not part of the ACA, many cite it as helping improve care quickly for those that are able to access the benefit). She shared results of a Kaiser Family Foundation survey that emphasized the need for ACA provisions:.png)
Whole-Population Interventions Aim to Prevent Type 2 Diabetes
As type 2 diabetes rises in the United States (and around the world), organizations are working to prevent new cases and improve the health and wellness of entire communities. Simon Neuwahl (RTI International) showed models of the benefits of proposed changes, which includied soda taxes, worksite health promotion, and bike lanes. The models suggest that the introduction of these three societal reforms can reduce the rate of type 2 diabetes by 17% over the next ten years. In 2018, 1.4 million people were diagnosed with type 2 diabetes in the, US so a 17% decrease would prevent 2.4 million cases over ten years.
There is still a long way to go. The CDC is aiming for the rate of type 2 diabetes to drop by 21% by 2025. The efficacy of some reforms, like the soda tax, are well proven. But, experts like Professor Nicholas Wareham (University of Cambridge, England) believe that no single intervention can make a difference. Decreasing rates of type 2 diabetes will require societal and individual lifestyle reforms.
Thankfully, diverse groups recognize the need for holistic approaches to diabetes prevention. The CDC’s National Diabetes Prevention Program coordinates with both public and private organizations to connect people with diabetes or prediabetes to lifestyle change resources and programs. Neuwahl’s cost-effective model is adaptable to national, state, and local communities hoping to implement whole-population interventions. Together, his three proposed population-level reforms could directly improve the lives of 2.4 million people.








